The Interstitium
About five years ago, there was an explosion of science reporting on a “newly discovered organ” called the interstitium. It’s a network of fluid-filled spaces surrounding tissues and organs. How new this is disputed since medical knowledge has known and educated physicians about interstitial fluid for a long time (certainly since before the article was published in 2018). Its status as an organ was also in dispute as that may have been more a product of public relations than the conclusions of the original article. However, while the authors responsibly represented their findings in the original article, the press was more willing to make outrageous connections and claims. There was an infamous Science Friday interview in which they claimed that the interstitium basically explains how and why acupuncture works (spoiler alert: it doesn’t and it doesn’t). Ditto in an interview with The Cut. More recently, the popular WNYC show Radiolab did an episode on the interstitium that was also quite friendly to the ideas espoused in those other interviews.
Interstitium vs Fascia
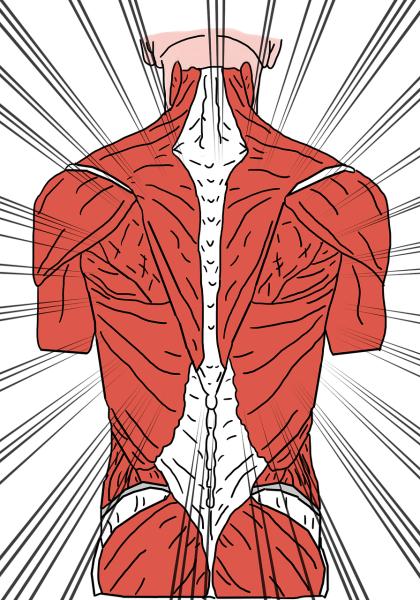
The idea that a unifying bodily organ, system, or force exists on which health status hinges is not new; in fact, this is what the doctrine of vitalism espouses. Some call this “unifier,” fascia, a buzzword in some alternative medicine circles, e.g., chiropractors. According to SpinalCare.com, a chiropractic website,
“Fascia is a thin, slimy covering that surrounds every muscle, tendon, ligament, and organ in the body. The fascia provides a friction-free surface for internal structures to move without abrasion or damage.”
You aren't alone if you think this sounds a bit like the interstitium. According to Neil Thiese, one of the authors of the original study of the interstitium,
“Nomenclature is an issue: If you focus on the connective tissue, you call it ‘fascia’; if you focus on the fluid, it’s ‘interstitium.’ We have a lot of talking and work to do across disciplines to sort this out.”
The point is none of this is new—only our understanding of how the interstitium works has changed. Chiropractic, Rolfing, and osteopathic manipulation have all based entire belief systems around the existence of a grand “unifier,” however, the interstitium and fascia are not that grail. Let’s dig into some evidence around these modalities.
Chiropractic
Chiropractic manipulation was created by Daniel David Palmer in 1895 based on the idea that relieving obstructions in nerves via manipulating the spine (mostly) promoted health and healing. The idea is that displaced vertebrae and general joint dysfunction place pressure on nerves and can influence other areas of the body. By correcting that, you can cure almost anything. But how, you might ask?
The answer is that fascia connects everything in your body, so if you can manipulate them and relieve those obstructions, you promote health and healing within the body…that’s according to the chiropractic theory of subluxation. Back pain has become the number one condition for which chiropractors will tout their theory and success in treatment, but it quickly falls apart the minute you venture into the realm of evidence.
A 2009 epidemiological examination of evidence for causation, published in Chiropractic & Osteopathy, concluded that,
“No supportive evidence is found for the chiropractic subluxation being associated with any disease process or of creating suboptimal health conditions requiring intervention. Regardless of popular appeal this leaves the subluxation construct in the realm of unsupported speculation. This lack of supportive evidence suggests the subluxation construct has no valid clinical applicability.”
In 2011, a Cochrane Review article concluded
“[h]igh quality evidence suggests that there is no clinically relevant difference between spinal manipulation therapy and other interventions for reducing pain and improving function in patients with chronic low-back pain.”
If the fascia and the “new” interstitium functioned the way that subluxation theory claims they should, we would have seen something in the literature by now, and we have…it’s just the exact opposite of what this theory claims. Even in the realm of back pain, it seems this theory falls well short of the mark regardless of any “discovery.”
Osteopathic Manipulation
Osteopathic manipulation (OM) is based on the idea promoted by Andrew Taylor Still that manipulation of the spine and bones improves blood flow and health by allowing the body to heal itself. It is related to chiropractic in that they both came from the same region in the United States in the late 1800s and focus on the musculoskeletal system as the locus of health. Again, you may find yourself asking how this may be the case. Fascia (and the interstitium), of course!
The most significant victories OM claims are treating lower back pain (similar to chiropractic) and the Spanish Flu pandemic. Having already discussed chiropractic, we’ll focus on the bigger claim pertaining to the Spanish Flu.
An often-cited osteopathic statistic is that during the Spanish Flu pandemic, those under the care of DOs (as opposed to MDs) had a much lower death rate. (0.25). This skirts the fact that this number is based on entirely self-reported data and a biased sample of DOs voluntarily submitting data. There was no accounting for those DOs that did not submit data and no verification of those that did. As a result, the belief persists that OM can treat pneumonia and influenza, which often results in pneumonia. For example, consider this article on the benefits of OM during the 2012-2013 influenza season or this review in the Journal of Osteopathic Medicine. Many osteopaths also promote the use of vaccines in addition to the use of OM. Still, using one well-documented prophylactic does not excuse the advocacy of a useless treatment. If the interstitium and fascia worked as OM theory claims they do, it would have revolutionized medicine and healthcare. Alas, OM can only claim minor victories.
To the credit of doctors of osteopathy, roughly 6% use OM techniques with patients, and as a result, the field is having a bit of an identity crisis in separating itself from medical doctors. For my money, DOs are basically just as good as MDs…as long as they leave the OM back in osteopathic school.
Rolfing Structural Integration
Created by Ida P. Rolf based on her belief that fascia surrounds all tissue and bodily structures; therefore, fascial manipulation can affect all underlying structures and tissues. According to the Dr. Ida Rolf Institute,
“More than fifty years ago, Dr. Rolf recognized that the body is inherently a system of seamless networks of tissues rather than a collection of separate parts. These connective tissues surround, support, and penetrate all of the muscles, bones, nerves, and organs.”
This led to Rolf developing a series of 10 treatment sessions and goals, ostensibly focusing on breathing, posture, spinal elongation, leg stability, the balance of the trunk over the legs, pelvis and lower extremity stability, balance and rhythm of head movements, lower-body integration, and upper-body integration. This theory and treatment have influenced proponents of OM and chiropractic alike, and you can easily see why the interstitium has Rolfing proponents excited.
However, like chiropractic and OM, if the interstitium and fascia worked in the way proposed by Rolf, we would have seen evidence of this. Instead, Australia, after conducting a thorough review and a call for evidence of effectiveness, has removed health coverage for this treatment. Evidence of efficacy was hard to find because there is little published research on Rolfing. Even the friendly-to-the-idea Journal of Alternative and Complementary Medicine published an article concluding,
“Evidence for clinical effectiveness and hypothesized mechanisms is severely limited by small sample sizes and absence of control arms. In view of the rapidly increasing availability of SI and its use for treatment of musculoskeletal pain and dysfunction, more adequate research is warranted.”
Ouch! When a friendly journal publishes an article admitting that evidence is scarce, primarily anecdotal, and lacks control arms, that’s pretty telling.
Where This Leaves Us
Given the abundance of alternative medicine theories and treatments claiming vitalism as an essential part of their belief system and the amount of time, money, and effort we have devoted to research, we would have found some consistent indication that this theory is correct by now. Regardless of a “newly”-not-so-newly discovered “organ” that tickles the senses of proponents of these modalities, the fact remains that these therapies don’t work. It’s fine to have a theory, but if the theory does not hold up to scrutiny, it’s time to change that theory.
Given the relatively new discoveries about the interstitium, the theory of cancer metastasis is evolving. Given the evidence and new discovery, Will Rolfing, chiropractic, and osteopathy change? My guess is no. Despite an overwhelming lack of evidence, they’ve proven resilient. Once stuck in the 1900s, always stuck in the 1900s…