As the Proposed National Ambient Air Quality Standards for Particulate Matter writes,
"Scientific evidence shows that long- and short-term exposures to PM2.5 can harm people’s health, leading to heart attacks, asthma attacks, and premature deaths."
There are several problems with this concept:
- Only long-term effects are at issue since no changes are proposed to the short-term (24-hour) standard.
- What happens in the short term is part of what is experienced over the long term and will become relatively more important if the new standards are implemented.
- The constituents of PM2.5 that might be inhaled and then affect the cardiovascular system comprise a minuscule fraction of typically measured PM2.5 and are unlikely to be controlled by the proposed regulatory action.
- The purported “evidence” solely comprises observational statistical relationships, but empirical test results are required to provide evidence. Individuals whose lives may have been shortened or extended in response to changes in air quality have never been identified under current conditions.
To be fair, EPA is faced with an impossible research problem. “Evidence” requires imposing a condition resulting in the purported effect, then removing it and retesting to see if the effect is relieved, which is not an option here:
- Because of its myriad sources, ambient PM2.5 exposures cannot be reduced sufficiently for experimental purposes.
- Indoor and, thus, total exposures cannot be controlled uniformly.
- Such exposure gradients would have to be maintained for decades to evaluate truly long-term effects.
- The subjects of such experiments should include susceptible persons, which would be unethical.
What to do? History has provided some horrific air pollution episodes that comprise empirical testing by comparing the outcomes of survivors with those who were not exposed. These follow-up evaluations were performed up to 10 years after the events, long enough for long-term effects to have developed.
The Donora Fog episode
Donora, Pennsylvania, was hit with a 4-day dense fog in October 1948 that trapped fumes from local industry, including a zinc smelter. From the population of about 12,500, 20 died during the four days, about 2400 were sickened, and many animals died. No environmental data were available during this episode, but particulate levels were estimated at 3000 µg/m3, and the fog penetrated indoors. The US Public Health Service conducted an extensive follow-up study to better understand this event by comparing subsequent mortality rates of survivors with and without fog symptoms, including residents of other areas.
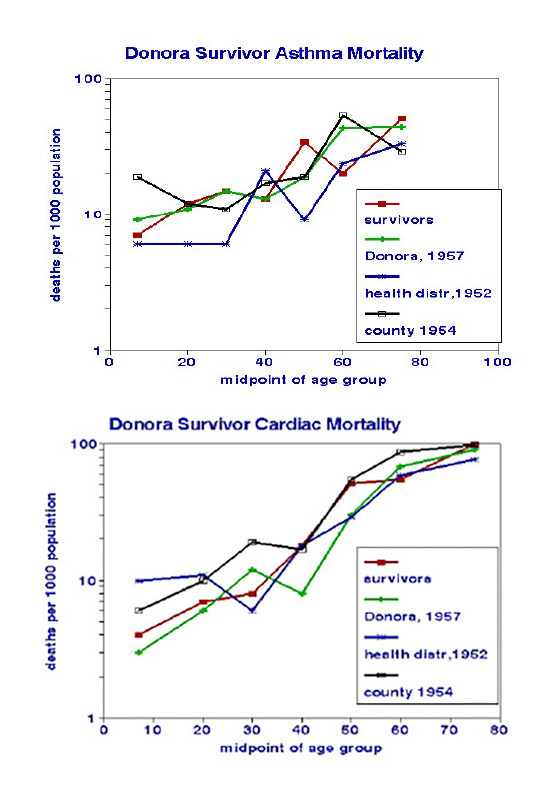 The graphs compare mortality rates for heart disease or asthma and age groups for four independent sub-populations: Donora residents affected by the fog, those unaffected, and individuals in the surrounding health district and county.
The graphs compare mortality rates for heart disease or asthma and age groups for four independent sub-populations: Donora residents affected by the fog, those unaffected, and individuals in the surrounding health district and county.
Visual inspection indicates no consistent differences among the four groups; statistical analysis shows a slight cardiovascular advantage for the non-Donora residents. The most important finding is the absence of an ongoing mortality penalty as the fog survivors age. The study also showed the importance of trends in smoking habits.
“No substantial or consistent relations between environmental and health experience could be demonstrated.”
A corollary is the absence of long-term health effects among the survivors of this horrendous episode.
The Hazelton Coal Mine Fire
A coal mine fire in Hazelton, Australia, lasted six weeks in 2014 and caused nearby PM2.5 exposures up to 3700 µg/m3.[1] Health studies included contemporaneous time-series analyses and comparisons of exposed with unexposed communities four years later. The National Library of Medicine database lists 23 Hazelton papers; most reported scant or weak fire-related health relationships, notably with cancer, COPD, or vascular causes. In time-series analyses, Dimitriadis et al. reported injury but not respiratory deaths associated with PM2.5. Other daily studies showed fire-related increases in medical service usage, medication dispensing, and lagged hospital admissions for respiratory and all causes. A wide variety of significant longer-term effects were reported from the 4-year post-fire analyses: psychological endpoints including post-traumatic stress, respiratory symptoms, fetal maturity, and diabetes. Associations with cardiovascular endpoints were not reported on any time scale. This list of health endpoints resembles a significance-shopping wish list.
The most important finding from the Hazelton fire is the absence of cardiovascular effects despite the extraordinarily high PM2.5 levels over a 6-week period.
Travel to New York City
A unique study of ischemic heart disease in New York City (NYC) provided some insights into urban contrasts. They considered being in the city a source of stress, which I assume would include air pollution exposure from traffic. The outcome variable was deaths from 1985-94, which would qualify as long-term exposure. The statistic of interest was the ratio of observed to expected death rates. I assumed relative exposure times based on hypothetical residence periods. Note that ambient air quality was nearly the worst in the nation in 1985-94 (PM2.5~ 20 µg/m3).
 Long-term residents and visitors had similar mortality risks at about twice that of residents who relocated before the mortality observation period. Although confounding may be an issue, these findings are consistent with short-term effects while in the city, with minimal after-effects. Such effects have been associated with traffic-related pollutants in various daily time-series studies.
Long-term residents and visitors had similar mortality risks at about twice that of residents who relocated before the mortality observation period. Although confounding may be an issue, these findings are consistent with short-term effects while in the city, with minimal after-effects. Such effects have been associated with traffic-related pollutants in various daily time-series studies.
Summary of the “experiments”
These three studies, like hundreds of others dating back to 1971, found short-term air pollution associations with mortality. However, they may be unique in their evaluations of survivors after a decade. They found no evidence of lasting impairment, consistent with the short-term frailty hypothesis and loss of homeostasis supported by animal experiments. Short-term effects may contribute to annual mortality rates, but they do not support air pollution as a cause of incident cardiovascular disease, on which EPA’s long-term standards have been based.
A key concept in the philosophy of science is that a valid theory must be capable of “falsification” no matter how much supporting data has been accumulated. The EPA’s no-threshold theory that any exposure to PM2.5 can cause heart disease is refuted by these 3 real-world examples. The studies supporting EPA’s previous regulatory actions were all observational, i.e., based on populations rather than individuals. Most of them were unable to adequately control confounding, and none considered indoor air quality. The price of imposing a stricter PM2.5 standard should be establishing a new ongoing observational study in which affected municipalities are compared with the rest of the nation as their air quality improves.
In plain language, the EPA should
Put up or shut up!
[1] Emissions from the coal mine fire were notable for not including metals, sulfur, nitrogen oxides, organic carbon, oxidants, and internal combustion engine exhaust, including diesel.



