Moral Hazard
When applied to economics, the term "moral hazard" refers to the incentive to use services you do not necessarily need because the cost to you is low or even free. Prior authorization (PA) is the means that insurance companies use to prevent the sin of overuse. Let me give you a quick example. In vascular surgery, removing varicose veins requires prior authorization. Insurance companies will pay for their removal when it is medically necessary, but not for cosmetic reasons. To have insurance pay for this treatment, as the physician, I must document through prior authorization an underlying abnormal physiologic condition using ultrasound and that the patient has been instructed and has presumably complied with wearing compression stockings for three to six months. If those conditions are met, the surgery and payment are approved. The requirement to wait those six months wearing compression stockings is often a sufficient hassle for those with primarily a cosmetic interest to forego the procedure or pay out of pocket – reducing insurance expenditures and preventing the moral hazard.
The Current Study
The Kaiser Family Foundation reviewed data collected by the Centers for Medicare and Medicaid Services (CMS) on Medicare Advantage programs -- what CMS calls Part C. I’ve written countless times about these programs, which seem to be primarily an advantage to the insurer, but are rapidly growing and overtaking the number of traditional Medicare beneficiaries.
The dataset includes 87% of Medicare Advantage enrollment, 23 million beneficiaries. In 2021, prior authorization was requested 35.2 million times – 1.5 requests for each and every beneficiary. Prior approval is most often required for high-cost services, like cancer therapy, the increasing use of biologicals, and post-hospitalization care to hasten recovery. Of course, not all beneficiaries had services requiring PA, and the requests for PA varied considerably among the insurers – from a low of 0.3 requests per beneficiary from Kaiser Permanente to nearly three requests per beneficiary with Anthem. The variability is a complex function of:
- How ill the beneficiaries may be in any given Medicare Advantage plan
- Restrictions that these plans provide to prevent the moral hazard of their spending money “unnecessarily.”
- Providers exempt from prior authorization “with a history of complying with the insurer’s prior authorization policies.”
The Power of No
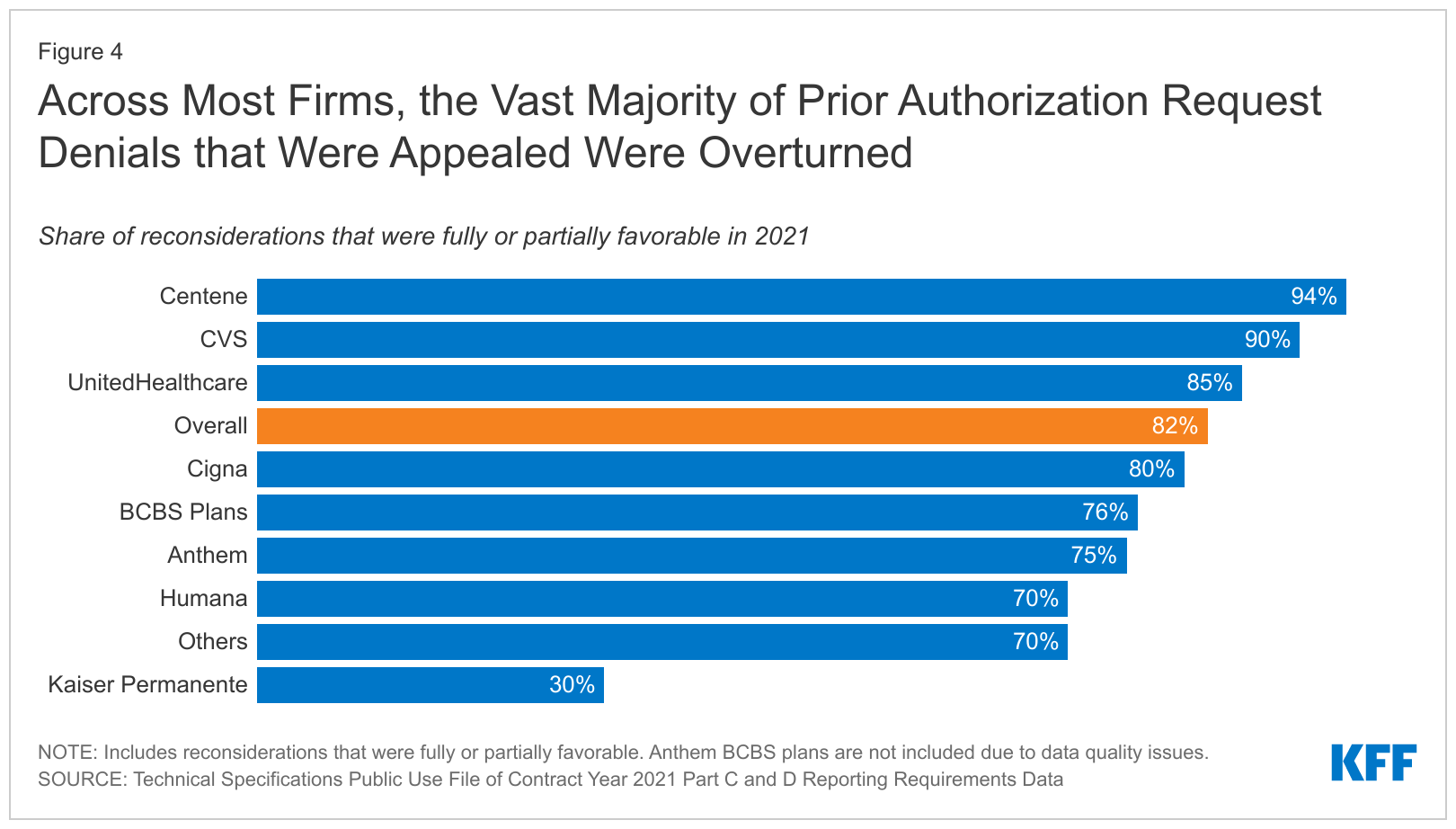
Of those 35 million PA requests, two million, 6%, were denied. And here is where the power of PA in preventing moral hazard lies. Only 11% of those denied claims were challenged. On average, 80% of those challenges were decided in favor of the beneficiary, allowing the care. Simply saying no, just once, eliminated requests.
But if 80% of the appeals are overturned, are the reasons for PA applied appropriately to medical needs? Or is the documentation required unclear or a hurdle of its own?
The power of no has an additional feature, an asymmetry of effort. To obtain a prior authorization, physicians must provide documentation from their records and tests – all work performed by their staff, all uncompensated, and all taking time. To deny a prior authorization requires about one minute of an insurer's time. To appeal a denial takes additional time, always more on the provider's side than the insurer's. It is a hassle to get PA, which is why it is a form of “rationing by hassle,” like the long lines at the DMV or those long wait times on the phone because “we are experiencing greater than expected call volume.”
CMS has proposed a rule that would hasten conversion over to electronic PA processes, at least reducing the time on the phone and, if the large electronic medical records companies join in, automating the process of connecting PA requests with the necessary imaging information. It would also improve the timeliness of those decisions.
“…little is known about the implications for enrollees, including delays in treatment or differences in the criteria used in making coverage decisions.”
The data didn’t include information that would be helpful going forward, especially because Medicare Advantage positions itself as better than other Medicare coverage by its marketing and branding. Knowing what services were denied, the criteria for those denials, the delays imposed, and patient outcomes would be good. And that information should be in a format that a patient, acting as a consumer in purchasing a Medicare Advantage plan, can use to compare their needs to what is being offered -- in order to avoid surprises in coverage or lack thereof!
Source: Over 35 Million Prior Authorization Requests Were Submitted to Medicare Advantage Plans in 2021 Kaiser Family Foundation




