Maybe I got it wrong, and the real point of the article was to “debunk” the value of cannabis in the treatment of pain. But the role of media attention in creating an expectation for cannabis pain management is in the title and the study’s objectives, so why not give those findings equal prominence?
A bit of background
Before jumping in, let’s look for a moment at the use of cannabis in pain management. A study in JAMA Network Open sought to characterize why cannabis products were purchased for medical use in New York. From January 2016 to August 2019, roughly 27,000 patients purchased 80,000 formulations of cannabis. These medical users were slightly more female and older than 50. The top three “conditions or symptoms,” severe pain, chronic pain, and neuropathy. [1] Dosages ranged from 2 to 10 mg, although “patients in all age groups...preferred high THC products.”
There can be little doubt that these patients and their physicians see cannabis as an effective tool in pain management. That is not to say that they deliver the same relief as opioids (assuming you can obtain them legally), but at least cannabis is considered adjunctive care. The percentage of individuals finding sufficient relief with cannabis itself is unknown, as are the numbers of individuals self-prescribing cannabis.
Cannabis Meta-analysis
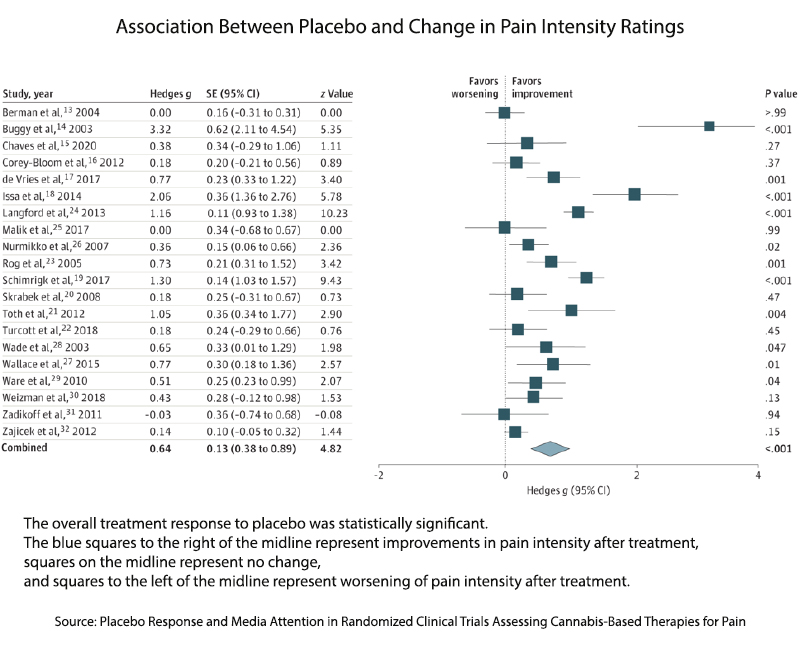
“Although patients improve in double-blind, placebo-controlled trials, there is limited superiority of cannabinoids over the placebo response, which suggests that the placebo response contributes considerably to the pain reduction seen in cannabinoids in clinical trials.”
There it is, the central belief being considered. The cannabinoids are just a statistical significance better than placebo. To support this belief, the researchers considered studies comparing cannabinoids and placebo for their reduction in self-reported pain intensity. [2] They identified 20 studies that met their criteria and based their findings on them. Overall the studies involved about 1500 patients receiving a range of cannabinoids, including CBD. In many ways, these patients were similar to those in the background study I cited.
Here are the study’s findings as voiced by the lead investigator in his summary for The Conversation.
“Our meta-analysis showed that pain was rated as being significantly less intense after treatment with a placebo, with a moderate to large effect depending on each person. Our team also observed no significant difference between cannabis and a placebo for reducing pain.”
The collected studies were a bit of a hot mess. Study durations varied from a few hours to 3 months, the preponderance of studies involved neuropathic pain (a smaller subset of patients using cannabinoids for pain management), and the study sizes were, with three exceptions, generally small.
 Overall, I would characterize the studies as a bit “iffy,” not determinate of the impact of cannabinoids on pain; at best, they seem to be as good as a placebo. As a physician, I would have moved on to other interests; as a “health communicator,” I would not have reported on any of the studies. But that is just me.
Overall, I would characterize the studies as a bit “iffy,” not determinate of the impact of cannabinoids on pain; at best, they seem to be as good as a placebo. As a physician, I would have moved on to other interests; as a “health communicator,” I would not have reported on any of the studies. But that is just me.
The Role of Media – Did they bury the lede [3]?
To look at the role of media, the researchers began with each study’s Altmetric score. The Altmetric Attention Score is an algorithmic measure of the attention an article receives. You can find the weighting system here. Making the news is a BIG DEAL. There is no upper limit to these scores, especially an article that has gone “viral.” But generally, a score of 20 or greater is considered good.
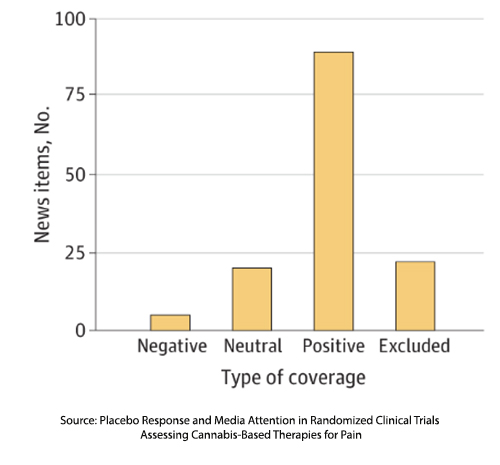 The mean score of the studies in the meta-analysis was 86, but this fails to separate academic attention from media attention. To get at the media role, the researchers identified 136 news items associated with the studies, characterizing them as positive, neutral, or negative concerning the role of cannabinoids in managing pain. Most of the media coverage was positive concerning the role of cannabinoids in treating pain.
The mean score of the studies in the meta-analysis was 86, but this fails to separate academic attention from media attention. To get at the media role, the researchers identified 136 news items associated with the studies, characterizing them as positive, neutral, or negative concerning the role of cannabinoids in managing pain. Most of the media coverage was positive concerning the role of cannabinoids in treating pain.
“We can conclude that these articles receive considerable attention in the general media. Furthermore, this attention is independent of how biased the study is, how high the placebo response is, or how low the treatment effect is.”
There you have it, media coverage, irrespective of the study’s results, were positive. This is not good science journalism.
The placebo effect is strong and should not be ignored. Roughly 30% of people will, given the proper context and encouragement, find that a placebo works as well as an active agent. Placebos are powerful tools in the medical toolkit. The question being asked, the lede being buried, is the media's role in creating expectations.
The medicinal role of cannabinoids is an attention-getting issue, entangled as it is with increasing legalization and cultural do’s and don'ts. So, it is no surprise that the media covers these studies. It is disheartening that they cover the findings so poorly. But as the researchers point out, “reports in the mass media and lay press and information obtained from the internet foster treatment expectations.” And those treatment expectations, in turn, may introduce bias into placebo-controlled studies, but more importantly, into the perceptions of regulators and policymakers.
“…positive attention regardless of effect size or risk of bias could have far-reaching influence on clinical trials, regulatory decisions, clinical practice, and ultimately patient access to cannabinoids for pain relief.”
Journalism can do better, and so can science-curious readers. Here is a reasonable guideline, you can safely ignore an article reporting on a scientific result if it doesn’t link to the study itself.
[1] Neuropathy, an abnormal response by sensory nerves, can cause numbness or increased pain.
[2] They did not consider the impact of cannabinoids on patients’ quality of life or pain’s impact.
[3] The lede is the opening of an article, summarizing the essential aspect. It is an older form of “clickbait.”
Source: Characterization of Cannabis Products Purchased for Medical Use in New York State JAMA Network Open DOI: 10.1001/jamanetworkopen.2022.27735
Placebo Response and Media Attention in Randomized Clinical Trials Assessing Cannabis-Based Therapies for Pain JAMA Network Open DOI: 10.1001/jamanetworkopen.2022.43848




