Ocular melanoma is a form of cancer that begins, most commonly, in the uveal layer of the eye that forms the capsule of the eye just below the sclera, or white portion. The choroid is the largest portion of the uveal layer, lying just below the retina, where most ocular melanomas arise. While they share the name melanoma with 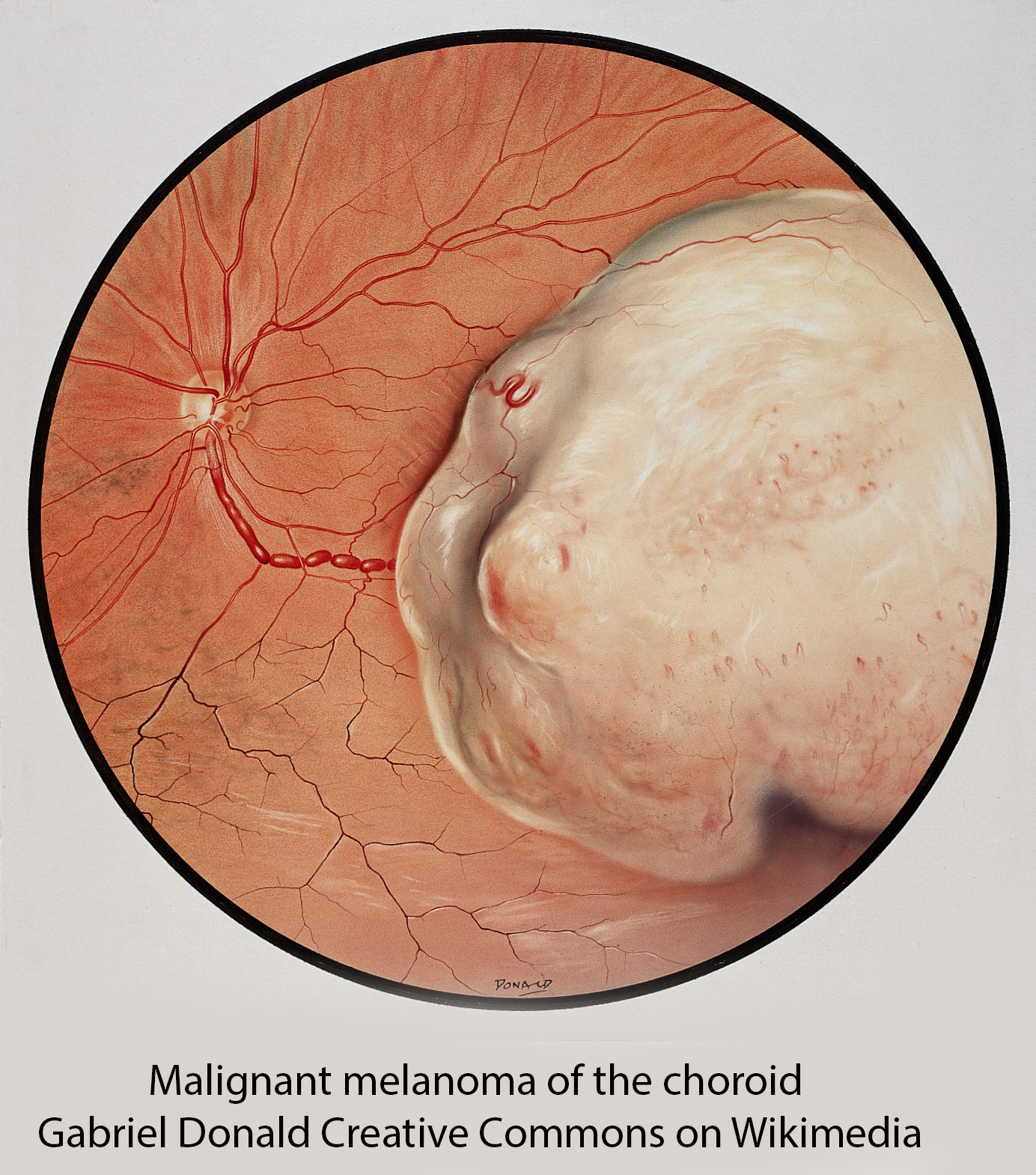 cancers of the pigmented tissue of the skin, they are very different biologically and genetically; they are also very rare, afflicting 5 out of 1,000,000 individuals.
cancers of the pigmented tissue of the skin, they are very different biologically and genetically; they are also very rare, afflicting 5 out of 1,000,000 individuals.
Ocular melanoma or OM is frequently asymptomatic, only causing symptoms of visual changes or pain as they grow larger. Those located less frequently in the front of the eye may present with a bulging of the eye, a change in the shape of the eye, or manifestations of increasing pressure within the eye.
We do not know what causes OM other than the common scientific belief that DNA abnormalities lead to malignant, uncontrolled cellular growth. While cutaneous melanomas are, as I said, different, both melanomas share similar risk factors, including fair skin, a propensity to sunburn rather than tan, and in the case of OM, light-colored eyes. Many skin changes, like atypical moles (dysplastic nevus syndrome) and atypical freckles, are conditions that increase the risk of OM.
Approximately 2,500 individuals are diagnosed with OM, with about 390 deaths annually, without gender or ethnic proclivity. It is 8-10 fold more common in Whites than those of African descent. Because it may be asymptomatic, a suspicion of OM may be made during a routine eye examination after one’s pupils are dilated and the inner eye examined. A more formal diagnosis can be made using ultrasound imaging or a dye (fluorescein) taken up by the blood vessels in the eye that detect a mass being fed by many blood vessels. More invasively, a fine needle can be placed in the anesthetized eye, and a tissue sample taken.
As with other malignancies, treatment of OM depends on its clinical stage, how aggressive the tumor appears, based on how abnormal its cells are, and whether it has spread outside the local area. Generally, the treatment options are the destruction of the tumor using radiation, applied locally or from an external beam, or surgical removal. As with many other cancers, biologics are also becoming therapeutic choices, specifically tebentafusp-tebn, which activates T-cells to enhance our immune response.
The prognosis, like the treatment, is stage-dependent. Those cases caught early have a five-year survival of 82%. When the tumor has spread locally, that survival drops to 71%. In the presence of distant spread, often to the liver, the five-year survival plummets to 13%.
Sources: Ocular Melanoma National Organization of Rare Diseases
Cancer.Net American Society of Clinical Oncology Eye Cancer: Statistics




