“…vaccines do not offer complete protection against infection by SARS-Cov-2…” Clinical Infectious Disease
For us, this is personal. One of us is entering his 10th decade with a large 3-generation family gathering – from Oregon to Scotland. We’re all vaccinated and boosted, but what about masking, crowding together, hugging, and kissing? Should I follow the science we just developed, call the whole thing off, or accept the risk and go for it? It’s complicated, but fortunately, I have six months to decide.
COVID-19 statistics [1]
- 24% of the population has been infected
- 53% of cases have been hospitalized. Of those, 19% were in ICU
- 1.2% of cases resulted in death
- 64% of our population has been fully vaccinated.
Using a national data set, we extracted weekly COVID-19 outcome data on about 150 million individuals by vaccination status; we focused on three age groups: 50-64, 65-79, and 80 and over. The fractions of vaccinated individuals increased to about 80% over the period, depending on age. Infections of vaccinated individuals were classified as “breakthrough” [2] despite having no information on the timing of their vaccinations - part of the original 2-shot series designated as “completed.”
The rates of infection (as measured by cases) followed similar temporal trends for both vaccinated and unvaccinated individuals. The summer surge is likely due to the arrival of the delta variant, with similar effects on both groups. There were no apparent age effects among the breakthrough cases and only relatively minor differences among the unvaccinated individuals. Case rates for the very elderly unvaccinated were about 50% lower than the “younger” cohort. This may reflect a survivor bias, the more frail having been previously “infected.”
By contrast, death rates showed strong age effects for both the vaccinated and unvaccinated. Age appeared to be more critical than vaccination status. Case fatality rates (CFRs), lagged by two weeks, showed a 10-fold greater mortality for the unvaccinated when considering age; and a 20 to 50-fold greater mortality for the unvaccinated, compared to those vaccinated with breakthrough infections.
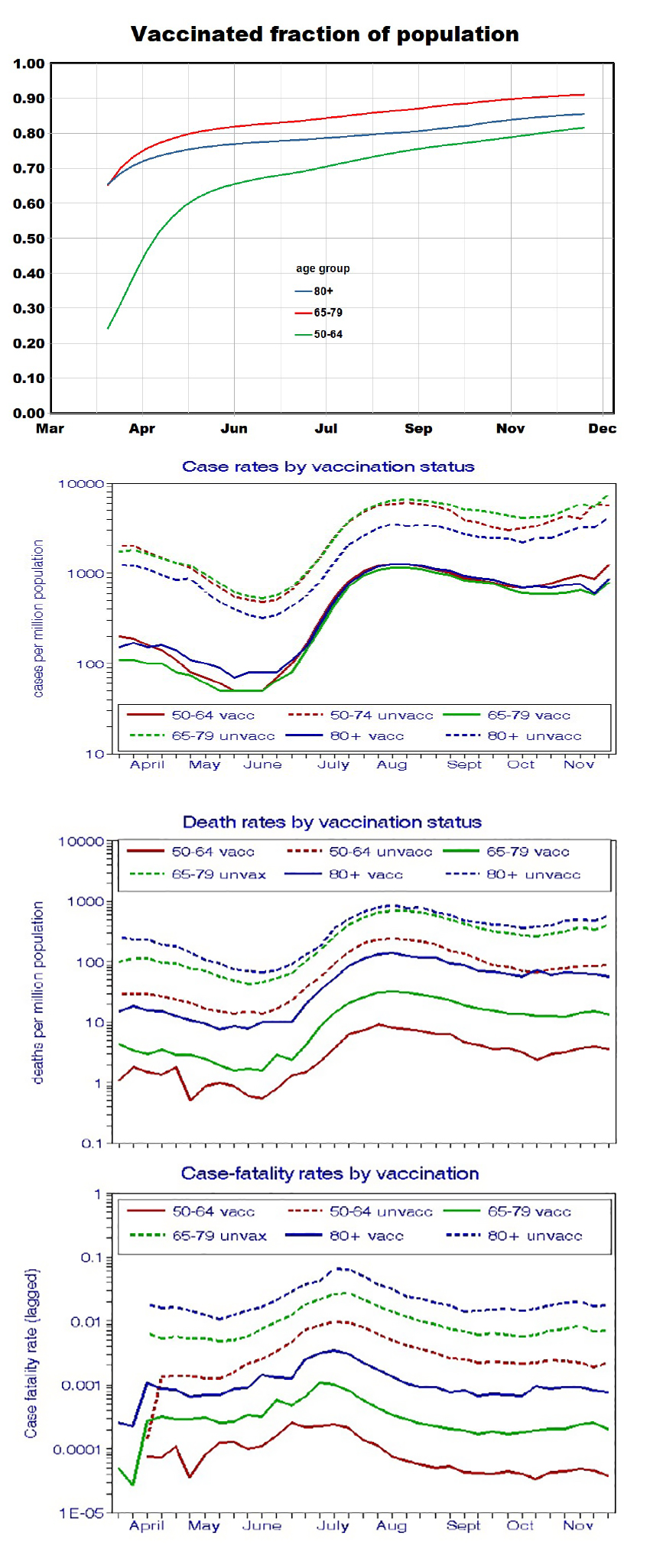 In July, there were strong increases in infection rates, mortality, and CFRs, the most crucial event in 2021, attributed to the delta variant. The surge affected the vaccinated more than the unvaccinated, thereby reducing the benefits of vaccination during the delta variant period:
In July, there were strong increases in infection rates, mortality, and CFRs, the most crucial event in 2021, attributed to the delta variant. The surge affected the vaccinated more than the unvaccinated, thereby reducing the benefits of vaccination during the delta variant period:
increases for the vaccinated increases for unvaccinated
- case rates: 20-fold 10-fold
- death rates: 12-fold 10-fold
- case-fatality rates: 5-fold 8-fold
New vaccination rates dropped to less than 0.1% per day in July, and the breakthrough ratio declined by half.
Much of our previous thinking attributed variations in COVID-19 outcomes to changes in vaccination rates, specifically the long decline in early 2021 and the substantial differences in cumulative rates among states. Our current analysis focuses on temporal trends stratified by age and vaccination status, such that vaccination rates per se are no longer an issue.
The graph shows parallel trends in new cases and vaccination rates for both vaccinated and unvaccinated subsets, which we did not anticipate. How could vaccinations have affected the unvaccinated? This question assumes that early reductions in COVID outcomes among the vaccinated were, in fact, due to previous increases in vaccination rates. The CDC reports also show these trends (without mentioning “breakthrough”), but they made no attempts to explain them. It seems clear that something else is going on, but what? A likely factor could be vaccinations decreasing the population’s viral load and reducing exposures for everyone.
An undesirable feature of this type of time-dependent analysis is the unavoidable change in the composition of the two population subsets during 2021, comprising an uncontrolled variable. It seems likely that the earliest vaccinators might have been those most in need, with the remaining unvaccinated comprising the most recalcitrant. As the pandemic progressed, the unvaccinated subset would become more vaccine resistant, on average.
This uncontrolled variation was not random. Our earlier state-level analysis indicates COVID outcomes correlated with socioeconomic and other differences between vaccinated and unvaccinated groups. That includes behavior dictated by personal beliefs and actions.
Are breakthrough infections due to waning immunity?
To consider breakthrough timing, we used data from Hong Kong that showed breakthrough cases delayed up to 6-7 months after vaccination. Since vaccinations began in January in the US, we expected breakthroughs to begin in Iate spring, by which time about half of the unvaccinated would have been vaccinated. If this subgroup comprised the most susceptible individuals, the average health of that group would have improved, leading to lower infection rates for the unvaccinated.
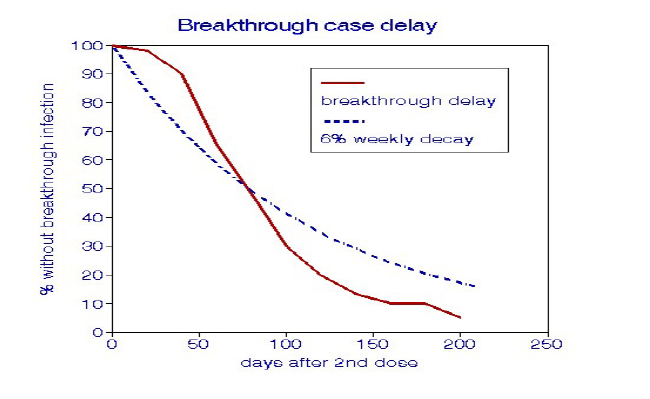
To consider whether breakthrough cases occur as antibodies diminish, we superimposed a progressive delay function of 6% loss per week on the Hong Kong data. It closely resembles the infection delays suggesting that previous vaccination was no longer as effective, with the variant held constant. We agree with an article on this topic published in the New England Journal of Medicine. Nevertheless, our demonstration that vaccination can confer benefits to everyone in the population, including the unvaccinated, seems noteworthy.
“Protection from SARS-CoV-2 …waned with increasing time since vaccination”
[1] As of mid-February, 2022
[2] The CDC definition of a “breakthrough” is an infection 14 days or more after vaccination.



