The first discussion of the disease that would later become AIDS appeared in an article in the June 5, 1981 Morbidity and Mortality Weekly Report (MMWR). Despite a massive effort by industry, academia, and government, the first drug to fight the virus, AZT (Zidovudine) was not launched until 1987. It certainly wasn't a cure. It was useless. (Except for extremely rare cases, AIDS has never been cured.) It is reasonable to call AZT a "treatment," since it was prescribed to AIDS patients, but it would be incorrect to call it a "therapy," since it wasn't helpful. AZT, the result of six-years of frantic research, failed to save a single life. There was no vaccine to prevent HIV infection at the time nor is there one today - four decades after the discovery of the virus.
It's wasn't until 1995 – 14 years after the beginning of the epidemic – that the death rate in the US began to decline when Roche introduced Saquinavir, the first drug that slowed the replication of the virus. The world had its first therapy for the infection. Dozens more AIDS drugs would follow over the next decade and AIDS became a manageable disease, much like diabetes, rather than a certain death sentence.
Since we have been bombarded 24/7 by coronavirus news, it should come as no surprise that a number of terms are carelessly being strewn about. Let's look at the terms "cure," "vaccine," and "therapy" as they apply to COVID-19; the disease caused by the "new" or "novel" coronavirus, aka SARS-CoV-2 (early on scientists called it the "Wuhan coronavirus" for the lack of any other term).
Three questions that now commonly arise are: "can we prevent it?", "can we treat it?", and "can we cure it?" The answers to these questions will also help you understand some of the terms – some used correctly, some not – that we are constantly hearing or reading about.
VACCINE – IS THERE ONE? WILL THERE BE ONE?
Of the three options, a successful (protective) vaccine would be the clear winner. It is better to prevent an infection than to treat or even cure it. In order to be treated or cured one has to be sick first. Given the horror stories coming from recovered patients, I'll take the vaccine any day (1).
The question "when will there be a vaccine?" is a bit presumptuous. No vaccine currently exists. That said, essentially every vaccine researcher in the world has coronavirus in his/her sights and they are sharing information and data rather than competing. This kind of cooperation is unprecedented and I think it will pay off. My best guess is that the chance of a successful vaccine is high. But this isn't always the case. Despite some very sophisticated advances in vaccine science and enormous efforts by immunologists, there remains no vaccine to prevent HIV/AIDS, herpes simplex, or hepatitis C.
WILL THERE BE A DRUG TO CURE THE INFECTION?
An antiviral drug can reduce the amount of virus present, the viral load, by thousands (often millions) of times. While this is the goal of any antiviral drug it is especially important with coronavirus because it is not that the virus itself that is the killer, but rather the overreaction of certain components of the immune system (especially cytokines) that plays a large part in the lethality of the infection. It can be (very) reasonably expected that when there are fewer infectious viral particles present the disease and the body's reaction to it will be milder.
In this case, "cure" is a matter of semantics. If a drug reduces the symptoms from severe (requiring hospitalization) to something more like a cold or bronchitis the body will eventually clear the virus and the infected person will regain his/her health. Did the drug "cure" the infection or did the body do so with the help of the drug? I doubt anyone will care.
CAN THERE BE A THERAPY THAT DOESN'T RESULT IN A CURE?
In the case of COVID-19, this is unlikely; a course of antiviral therapy should result in a cure one the virus is cleared and the patient healthy. But this is not always the case; some viruses are never entirely eliminated and the infection can return. For example, there are therapies for herpes and HIV and HSV, but no cures. For influenza, there is a vaccine (different every year), but it's not perfect (3) and a therapy that's worse (4). For those of you who become the unfortunate targets of norovirus ("stomach flu"), there is neither, although a number of companies have norovirus vaccine candidates in different stages of development.
BOTTOM LINE
The field of virology is fascinating but the rules can be complicated. In most cases, vaccines can be developed, but some viruses have refused to cooperate. By combining molecular biology with medicinal chemistry effective drugs have been developed, but this process can take many years. For example, there are now extremely effective (curative) drugs for hepatitis C, but it took 22 years for the first effective drug to hit the market.
Addendum
Here is a quick and dirty table showing some of the common viruses we face and how they can (or can't) be treated.
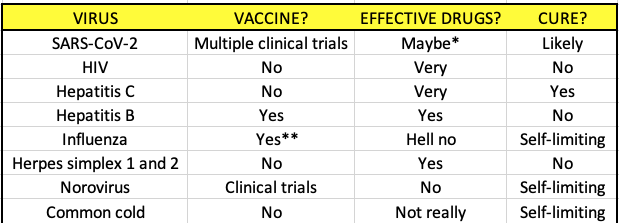
* As of the time of this writing only one drug, remdesivir, appears to be promising. Many more are being evaluated in multiple clinical trials all over the world. We will have answers soon.
** The flu vaccine is roughly 50% effective, however, this can vary widely from year to year. A universal flu vaccine, which would (presumably) be a single shot and offers protection for life is under development.
NOTES:
(1) Riddle: Q: What do you call an anti-vaxxer when a coronavirus vaccine becomes available? A: A hypocrite.
(2) The reservoir for herpes is nerve roots, for HIV it's CD4+ T cells (a type of white blood cell).
(3) The effectiveness of flu vaccines in the past decade has ranged from 19-60%.
(4) There are four approved flu drugs in the US. They range from bad to terrible.