Masks are two-way filters between the environment and your airway; they are a compromise between their ability to filter out particles and your ability to breathe. You will not inhale a single germ or virus if your mask consists of wrapping your head in "Saran Wrap," but of course, you will be unable to breathe and will suffocate. An N95 mask is >95% efficient at filtering particles of 0.3 micrometers. The droplets containing Covid-19 created when we talk, cough, and sneeze are roughly 5 micrometers and are kept out of lungs of the person wearing the mask.
Surgical masks are designed to protect the patient from health workers, specifically the patient undergoing procedures where body cavities are entered, with needle, knife, or tube, creating a heightened risk of you infecting them.
An N95 mask has two essential design principles. It must filter out those particles and must be appropriately fitted to your face. A moment of reflection will remind you how many shapes and sizes there are to the human face and that facial hair, like beards and mustaches, make a tight fit of the mask against your face difficult. "A fit factor is the number generated during quantitative fit testing by simulating workplace activities (a series of exercises, each 1 minute in duration)." A fit factor of 100 is required to approve N95 masks.
First responders and health care teams [2] are working in far closer proximity to infected individuals than you or I and, in many cases performing procedures that might expose them unintentionally to those droplets formed when patients cough and sneeze. That is why placing a breathing tube, and a host of other procedures require protection with an N95 mask. Following the CDC's standard precautions is adequate to protect the rest of us.
The need for N95 masks in the face of shortages has been written about in the scientific literature previously; in the instance, an article I am citing for avian flu in developing countries. Using a "Haynes Heavyweight 100% preshrunk cotton T-shirt," researchers made a DYI N95. The shirts were boiled, and air-dried, cut to size, and fashioned into masks [3]. Here it is.
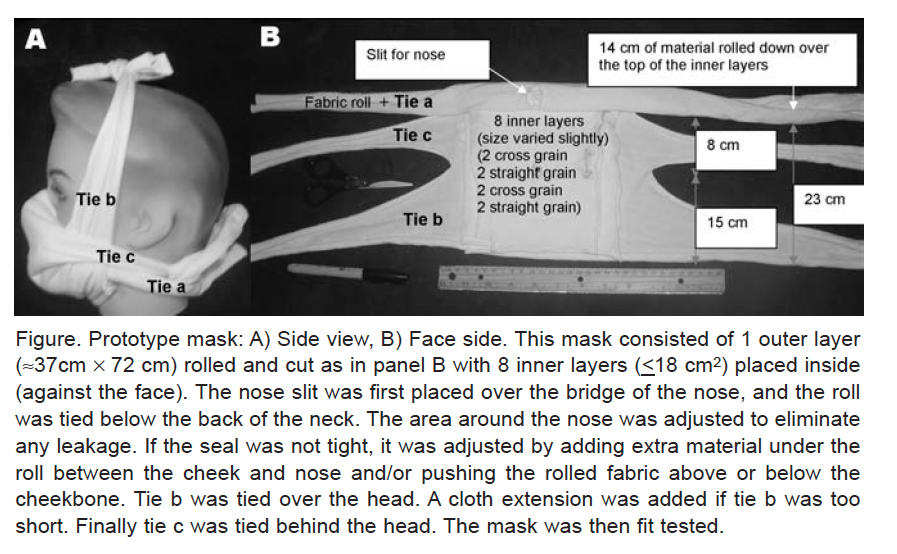
The best they could demonstrate was a fit factor of 67, with the two larger faces they tested having a fit factor of 13 and 17 – not overly protective. As the researchers report, while their DYI mask provided "a measurable level of protection from a challenge aerosol," problems remained. The bottom line, N95s are going to require design and manufacturing skills, like those of 3M, where production has increased two-fold since January to 100 million a month. If you are not a first responder or part of that healthcare army, you do not need an N95 mask.
CDC Standard Precautions
For the rest of us, consider the CDC's standard protocol for interacting with patients, irrespective of whether we know that they have an infection – just the circumstances the general public now faces.
- Hand hygiene – you should already know about washing your hands
- Gloves – when touching a patient or their bodily fluids. But "wearing gloves does not mitigate against the need for proper hand hygiene" after taking gloves off.
- Gown, Mask, Goggles/Eye Visor, and/or Face Shield – during procedures that spray or splash bodily fluids.
We, the general public, do not need protective gear; we simply need to wash our hands and observe that six-foot social distance. Those two standards have worked to protect healthcare teams for years against airborne aerosol droplets as long as they are followed.
The CDC guidelines go on to discuss additional precautions to be taken against airborne, droplet, or direct contact. Only airborne precautions require an N95 mask, and if you maintain a safe social distance, they do not apply to you. Droplet precautions require a surgical mask, not an N95, and again only when you are "within six feet of the patient." Are we getting the message?
As to direct contact, the CDC recommends gowns and gloves, but they are referring to direct contact with an infected patient, not the fear of those delivery boxes. Delivery boxes are never allowed in operating rooms nor upscale restaurants; the fear of unintended contamination is too high. How to best protect yourself is unclear from those delivery and take-out packaging. There is a suggestion that you leave them outside for 24 hours. Or you might do another reasonable thing, and wash your hands after opening them.
[1] a tracheostomy is placing a breathing tube through the skin of the neck directly into the trachea, intubation involves placing a breathing tube through the mouth following our natural passageways into the trachea. Neither is a project for amateurs other than McGyver.
[2] Healthcare is a team sport, and we should remember that it involves more than doctors and nurses; it includes respiratory, physical, and occupational therapists as well as individuals transporting patients, taking blood samples, bringing meals, and cleaning rooms.
Sources:
Simple Respiratory Mask Emergency Infection Disease DOI 10.3201/eid1206.051468
Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control DOI 10.1016/j.ajic.2005.08.018
Standard Precautions for All Patient Care CDC




