Although exhaustively studied, sometimes the immune system remains a black box. It has been harnessed in a number of different ways, most notably, in fighting cancer. While some results have been spectacular, there have also been some spectacular failures.
Recently, Juno Therapeutics Inc experienced the latter. The company's experimental leukemia drug, JCAR015, went down in flames last week after two patients in the clinical trial died from cerebral edema (swelling of the brain)—the same lethal side effects that were seen this past summer, when three other patients in the trial died. Not surprisingly, the company announced that it was putting the trial on hold.
JCAR015 is one of several experimental drugs called chimeric antigen receptor T-Cell therapy (CAR T) (1), some of which have shown promise in treating difficult leukemias.
It is difficult to see a path forward for JCAR015. Although the patients being treated suffered from a cancer that has a very poor prognosis, the fact that five patients died for the same reason indicates that something about 015 is fundamentally flawed.
This is not the first time that immune therapies have triggered unexpected responses during clinical trials.
In 2000, Wyeth (now Pfizer) and Elan, an Irish pharmaceutical company that primarily focused on therapies for Alzheimer's began a collaboration on bapineuzumab (2), an antibody that was designed to dissolve brain plaques.—the hallmark of the disease. At the time, there were high hopes for bapineuzumab, so much so that some stock analysts predicted that it could have sales of $13 billion annually. It turned out that they were off by only $13 billion.
This is because in 2008, 12 people who were being given the antibody developed a serious complication called vasogenic edema, a build-up of fluid in the brain. Although all 12 eventually recovered, Elan did not. The company closed up shop in 2013.
Another trial in particular is the stuff of bad sci-fi movies. So much so that the normally staid BMJ contained a paper in its March 2007 issue called “We saw human guinea pigs explode.” In 2006, in what can only be called a ghoulish catastrophe, eight unfortunate healthy volunteers (all men) were given a humanized monoclonal antibody called TGN1412 in a clinical trial at Northwick Park Hospital in London. TGN1412, like JCA015, was designed to target white blood cells. But, when the drug was administered, the volunteers quickly developed a cytokine storm, an extreme condition. The following quote from the Daily Star pretty much says it all.
“His head had swollen to three times its normal size. His neck was the same. It was wider than his head and his skin had turned a dark purple. At first none of us recognised him. His nose was spread across his face like it had been squashed. He had tubes in his nose and mouth and was hooked up to a machine helping him breathe and to a kidney dialysis machine. His eyes had been taped up and he had been sedated. Our fear is that he may never wake up.”
And, that was just one patient. Some of the others arguably suffered even worse, or at least gorier, consequences. Much of the blame for this horror show was due to errors by the investigators, in particular, dosing all the men one after another with no observation time, and continuing to dose after the first volunteers already developed symptoms.
"TGN1412: From Discovery to Disaster"—a review of the massive incompetence by investigators can be read here. But, not at the dinner table.
Notes:
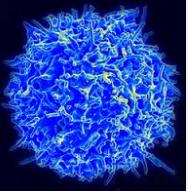
(1) T-Cell therapy involves removing T cells (one type of lymphocyte, which is a subset of white blood cells) from a patient, modifying their DNA so that the cells express different receptors on their outer surface. This enables the altered cells to zero in on and attack cancer cells. The modified cells are then infused back into the patient.
(2) I did not know of one single person in all of Wyeth who could pronounce bapineuzumab, so we called it "Bappy." Unfortunately, Bappy became Crappy.



