In the last few weeks, Stat posted its most recent article on their continuing investigation of United Healthcare, How UnitedHealth turned a questionable artery-screening program into a gold mine. At its heart, it is another expose of upcoding in Medicare Advantage programs – identifying medical diagnoses that contribute to the insurers' bottom line but offer little benefit to patients. As a vascular surgeon, I found the article particularly interesting and thought I might provide a little value-added commentary on Stat. 's already excellent work.
Peripheral vascular disease (PVD) refers to atherosclerosis of the arteries and has a similar pathophysiology and management as atherosclerosis of the heart. Metaphorically, vascular surgeons care for the pipes, while cardiologists care for the pump. In the lower extremities, individuals might find that blockages in their arteries cause them discomfort when they walk, relieved by a few moments of rest – that is claudication, the vascular surgery equivalent to cardiology’s angina. More severe cases can result in loss of tissue, a non-healing wound or gangrene, or cause relatively constant pain made worse when the limb is elevated (rest pain); again, in cardiology, these are equivalent to heart attacks. Atherosclerosis, a generalized condition, impacts all arteries, but the triad we most frequently see involves the vessels to the legs, heart, and brain. Having diagnosed an issue with one of these systems, the prudent physician will often search for asymptomatic disease in the others, if for no other reason than to begin more careful follow-up.
One of the beautiful qualities that attracted me to vascular surgery was the ability to diagnose peripheral vascular disease of the legs based on a simple history and physical examination. After asking about claudication and rest pain and searching the leg for non-healing wounds or gangrene, identifying pulses will establish the diagnosis. Other tests may quantify disease and provide numerical information to “follow.” However, that simple examination is often sufficient in the hands of vascular surgeons.
You might think that checking for a pulse in the foot is a simple exam. You, of course, would be wrong. Today’s examination in primary care often searches for a pulse with the patient wearing their socks or looking in the wrong place. I cannot tell you how frequently I have seen patients with pulses recorded when they are not present and absent pulses when they are bounding. Vascular surgeons have utilized the ankle-brachial index or ABI, where the blood pressure in the arm is compared to that in the foot, to quantify the risk of limb loss, making it a useful biomarker.
Suffice it to say that the ability to measure the blood pressure in the foot is not commonly practiced and involves more training and experience than measuring your arm's blood pressure. That is why the device deployed by United Healthcare, QuantaFlo, can be helpful. It eliminates inexperience and lack of training while providing a graphic output and report, similar to the ABI. When married with an appropriate history, it may help to identify those patients at risk of PVD.
United Healthcare applied that technology to a large, often asymptomatic population. QuantaFlo, as a screening test, yielded many false positives and negatives. I would guess it was no better than the cursory physical examination, but it could be mandated and documented in the ultimate billing algorithm, the electronic health record. The false positives all contributed to the upcoding that Stat reports increase the value of the beneficiary to United Healthcare by $3,600 annually.

That should go a long way in explaining this graph, which illustrates the widening gap in testing for PAD by those involved in Medicare Advantage.
Then, there is the issue of turf, although the term we use in medicine is scope of practice. Beginning in the 80s with the ascendency of angioplasty to treat coronary artery disease, there has been a similar rise in these non-invasive procedures to treat lower extremity arterial disease – remember, the treatments are very similar; it is the location and natural history that differ. At that time, the three specialties fighting over these patients were radiologists, who had pioneered the use of various tools and techniques to navigate the arterial system and treat disease non-invasively; vascular surgeons, who primarily performed open surgery on these patients but had specialized training in the natural history of PVD; and cardiologists, who were experienced in those tools and techniques for the coronary arteries and had patients who had both coronary artery and PVD.
The turf war continues to this day. Radiologists are often out of the equation; their work is primarily by referral, and they have never had their “own” patients. Cardiologists and vascular surgeons continue to snipe at one another, and admittedly, I am biased. There is a reason that I spent additional time caring for patients with PVD because they are similar but not the same as patients with heart disease. Cardiologists believing that one artery is just the same as another have been much later to the education party and now are offering add-on training in the care of PVD. The truth is, given that there are far more cardiologists than vascular surgeons and that coronary artery disease is more common than PVD, vascular surgeons have been slowly losing the war for years. Every expert cited in the Stat article was a cardiologist. My specialty didn’t garner a mention.
There is no doubt in my mind that United Healthcare deliberately upcoded charts; it is in the nature of a for-profit organization to turn a profit. But they took advantage of a situation they had only a small role in creating. They were not responsible for a good history and physical examination becoming more aspirational than actual. They were not responsible for reducing the hands-on physician moments to screentime. Nor were they responsible for the in-fighting of specialists over who gets the patients. They were responsible for deploying a screening test inappropriately.
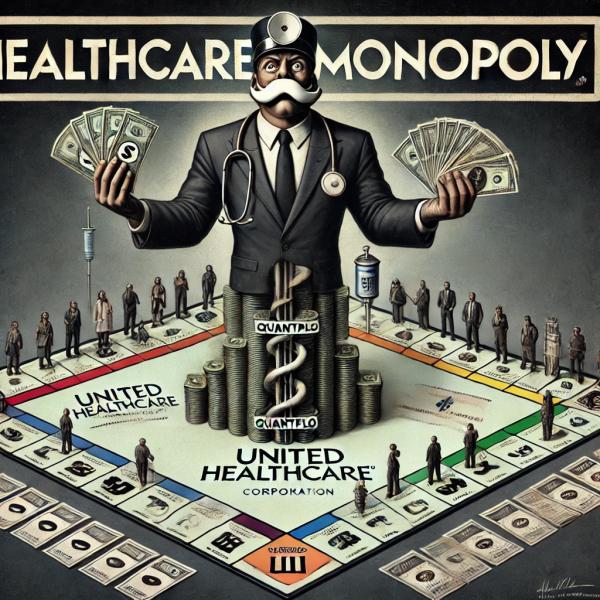
Calling United Healthcare out over this upcoding will not fix the problem. In a Darwinian sense, United Healthcare has shown its fitness over that of physicians and legislators in the healthcare space. The changes that may follow from this investigation will alter the environment. Still, I am betting that United Healthcare continues to be more savvy and agile than the other stakeholders.
UnitedHealthcare’s upcoding antics are just another symptom of a healthcare system where profit trumps patient care. However, this isn’t their first rodeo, and it won’t be their last. The Stat investigation might ruffle some feathers, but UnitedHealthcare is still king of the healthcare hill.



