Mental illness often responds to medication, but in turn, those medications may cause side effects that lead to suboptimal treatment or complete cessation of therapy. A pilot study suggests that a diet high in protein and low in carbs – a keto diet – may offer a helpful add-on treatment.
Neuroleptics, the general classification of medications used to treat schizophrenia and bipolar disorders, are effective. However, they have metabolic impacts in terms of weight gain and glucose dysregulation that make them problematic and contribute to an increase in early mortality in these patients, often from cardiovascular disease, compared to the general population.
“The relationship between metabolic dysfunction and psychiatric disease is likely multifactorial. Genetics, lifestyle factors, and medication have all been reported, to impact metabolic dysfunction in these conditions.”
The ketogenic diet replaces carbohydrates with fats, reducing the available glucose and providing an alternative fuel source; ketone bodies derive from fat metabolism. The Atkin’s Diet was an early form of a ketogenic diet and, for many individuals, resulted in significant weight loss. It seems that for some individuals with medication-resistant epilepsy, substituting ketones for glucose as the brain's primary fuel results in the reduction of seizures. That was among the metabolic “whispers” that led the researchers to this study.
This is a pilot study involving a small number of individuals over a short interval without a control group; it is intended to explore whether a more structured clinical trial is warranted. The 21 recruited participants all had established diagnoses of schizophrenia (5) or bipolar disease (16), were overweight, having gained “more than 5 % of body mass while using psychotropic medicines to manage their mental health condition,” and had some metabolic disorder – glucose or lipid dysregulation. All were placed on ketogenic diets, and several surveys and measurements were made over a four-month interval.
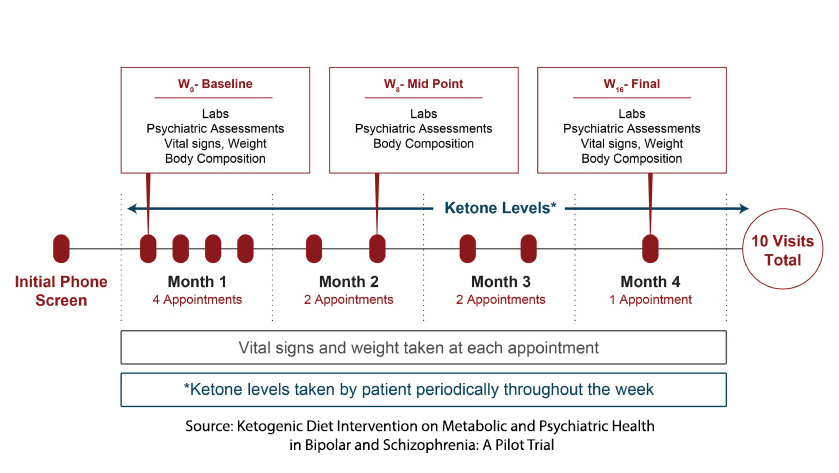 Using the measurement of ketone bodies as the criteria, 14 participants were fully adherent to the ketogenic diet; six were moderately adherent.
Using the measurement of ketone bodies as the criteria, 14 participants were fully adherent to the ketogenic diet; six were moderately adherent.
At the end of the four-month study:
- Average weight had decreased 10%
- Systolic blood pressure reduced by 6.5%
- BMI reduced by 10% and fat mass index decreased by 17%
These findings are consistent with expectations for a ketogenic diet. C-reactive protein, a marker of inflammation, and hemoglobin A1c were both reduced and, as expected with a diet high in fat, LDL and HDL values were elevated. There was no significant change in the calculated 10-year mortality from cardiovascular disease.
There was a small but notable 17-19% improvement in patient life satisfaction, functioning, and sleep. While 33% of patients were classified as “in recovery” at the beginning of the study, this increased to 75% by the end, and 100% of all participants who fully adhered to the study were “in recovery.” 79% of participants reported improvement in symptoms, which was greater among the most adherent.
“Taken together, our results show that a ketogenic diet intervention is a feasible and acceptable supplemental treatment to neuroleptic medications in an outpatient, real-world cohort, showing psychiatric and metabolic health improvements in those with bipolar or schizophrenia illness with co–morbid metabolic abnormalities.”
We can perhaps forgive the hyperbole of a “real-world cohort,” given that these were volunteers with an active interest in improving their lives and were not “blinded” to their treatment. But that having been said, it does offer new avenues of treatment and may, over time, counteract some of the metabolic tradeoffs required for the benefits of neuroleptic medication.
In summary, the pilot study suggests that a ketogenic diet be a beneficial supplementary treatment for patients with bipolar disorder or schizophrenia experiencing metabolic side effects from neuroleptic medications. More extensive, controlled trials are necessary to understand the potential benefits and limitations of incorporating a ketogenic diet into psychiatric treatment plans.
Source: Ketogenic Diet Intervention on Metabolic and Psychiatric Health in Bipolar and Schizophrenia: A Pilot Trial Psychiatric Research DOI: 10.1016/j.psychres.2024.115866




