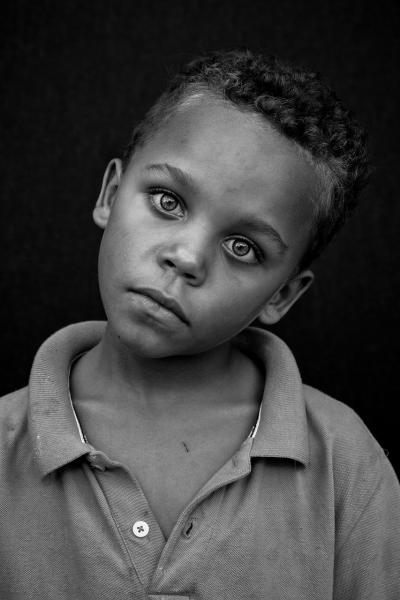
Glaucoma is both preventable, with early treatment, and the leading cause of blindness in those over 60. Additionally, the incidence of glaucoma and its harms are greater in both our Black and Hispanic communities. Before jumping to the always-present issue of “disparities,” let’s provide a little background.
A Glaucoma Primer
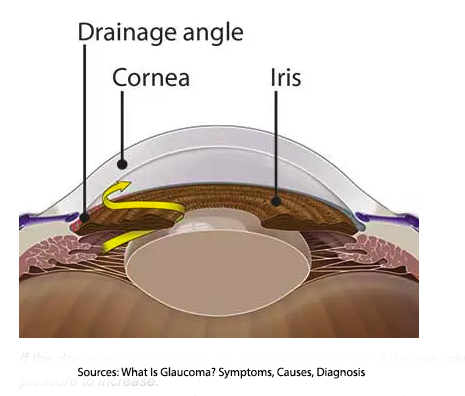 The shape of our eyeball, roughly a globe, is maintained by two fluids. In the front of the eye, as depicted in the image, there is aqueous humor, a clear fluid responsible for maintaining the proper pressure in the eye. Behind this area, between the lens and the retina, is the vitreous humor, a gel that provides much of that globular structure and nutrients to the eye.
The shape of our eyeball, roughly a globe, is maintained by two fluids. In the front of the eye, as depicted in the image, there is aqueous humor, a clear fluid responsible for maintaining the proper pressure in the eye. Behind this area, between the lens and the retina, is the vitreous humor, a gel that provides much of that globular structure and nutrients to the eye.
The aqueous humor is produced by ciliary bodies on either side of the lens (seen where the arrow begins), flows through the pupil, draining through a venous passage (the scleral venous sinus for those that must know) into the bloodstream. That flow helps to maintain a relatively constant intra-ocular pressure. When the pressure rises, it injures the optic nerve, killing the cells responsible for our vision.
When sufficient numbers have been lost, roughly 40%, we experience the symptoms of glaucoma, which include those impacting our vision, causing us to see halos or have decreased or blurred vision, as well as more non-specific findings such as eye redness, headaches or pain in the area of the eye. But this is late in the process; we have lost many of our visual cells before symptoms occur. While glaucoma is treatable, the damage it inflicts is not, which is why identifying an increase in intra-ocular pressure before it is symptomatic is crucial to glaucoma’s management.
Open-angle glaucoma is the most common form, impacting about 90% of patients, with a slow, indolent course, generally asymptomatic course. An elevation of the intra-ocular pressure is causative, but it is unclear what the underlying mechanism is that results in the reduction of drainage in the aqueous humor. Narrow-angle glaucoma results when the iris impinges on the drainage of the eye, again reducing outflow and increasing intraocular pressure. The onset of narrow-angle glaucoma may be chronic, in which case it presents much like open-angle glaucoma, or acute, with sudden changes in your vision and pain – a true eye emergency.
Tonometry is a diagnostic test for glaucoma and measures the pressure in the eye based on the eye’s resistance to being pushed on. While earlier versions of tonometry required prolonged “pushing” on the eye and applying a topical anesthetic, today’s tonometry involves puffs of air or microsecond contact with the eye, making it painless, quick, and non-invasive. It is a routine part of an ophthalmologic examination and is even done as part of the measurement for eyeglasses. An abnormal intra-ocular pressure identified at tonometry should lead to a more detailed examination of the retina, optic nerve, and optic angles.
A Silent Thief
Glaucoma, because it remains clinically silent for so long, results in 50% of individuals not knowing they have glaucoma. It is also a discriminating thief preying more on Blacks and Hispanics. As has been reported in multiple population-based studies, individuals of African descent have:
- Individuals of African descent have a six-fold greater prevalence of glaucoma, a similarly heightened incidence of blindness, and increased intra-ocular pressure 12 years earlier than other groups. For them, glaucoma is more rapidly progressive.
- Hispanics develop an acceleration of glaucoma after the age of 65, when the prevalence, until that point, equivalent to that of Whites, rises to that of Blacks.
- The prevalence of open-angle glaucoma in Blacks is 3.4%, for Hispanics 4.7%, and for Whites 1.7%. Demographic shifts will further alter the absolute number of individuals at risk over time.
Why the Disparities?
Short answer: it is multifactorial and unclear. How you weigh these factors depends upon the “lens” you apply – anatomic, physiologic, genetic, socioeconomic. In turn, that focus may suggest ways to improve care through enhanced access, screening, or more bespoke, personalized treatment.
- Anatomy - several anatomic features contribute to glaucoma. A thinner cornea may provide factitiously lower measures of intra-ocular pressure, and a larger optic nerve may signal a propensity for glaucoma – these anatomic differences appear more prevalent in Blacks. The larger iris may make it more likely to impinge upon the eye’s drainage.
- Physiology - It is a straightforward physiologic hypothesis that the elevated blood pressures within the Black community put them at increased risk for greater intra-ocular pressures. However, a study of Blacks in Barbados found that lower systolic blood pressures, not elevated ones, were associated with glaucoma. Of course, using the term Black to encompass a wide variety of ancestry makes these findings ambiguous.
- The physiology underlying the outflow of aqueous humor is poorly understood. Additionally, some anatomic differences in the structure of outflow tracts and optic nerve may create enhanced sensitivity to pressure changes.
- Genetics - A recent Genome-Wide Association Study (GWAS) involving 11,000 “individuals of African ancestry” identified 46 “risk loci” associated with open-angle glaucoma. Three of these loci were unique to the African dataset and were involved in reducing the outflow resistance from the eye. The derived polygenic risk score outperformed a similar score based on a genetic database of European individuals, suggesting that there was indeed a genetic element to the onset and rapidity of glaucoma in the population of African descent.
- Socioeconomic factors played a role, and a study demonstrated that lack of insurance, transportation, and education were all associated barriers to diagnosis. In a study of individuals attending a free eye clinic, a third of the missed appointments were due to a lack of transportation, and another third were due to “forgetting.” And that forgetting may be partly due to the absence of a spouse or family member. In the Advanced Glaucoma Intervention Study (AGIS), 56% of Blacks vs. 34% of Whites were never married, divorced or widowed. A lack of education, defined by the highest educational attainment or health literacy, also played a role. In a study of missed telemedicine care for glaucoma, 29.2% of “participants were unaware of or did not comprehend the severity of their ocular diagnosis.”
- Access to care is also an issue, made worse by the early and extended period of glaucoma’s harm to the optic nerve before becoming clinically significant. For a population that has difficulty accessing health care, an increased risk of asymptomatic disease results in less screening and contributes to the late diagnosis of glaucoma. A review of care provided to Medicare beneficiaries demonstrated that Blacks and Hispanics had less outpatient care for glaucoma and more inpatient, ED, nursing home, or home care visits than Whites. This was true for low and high socioeconomic circumstances, and this disparity in care was not seen for Asians – overall suggesting systemic and cultural components to seeking and obtaining care.
- Moreover, the same review indicated that Black and Hispanic patients underwent surgical intervention for glaucoma at higher rates than Whites. Whether this is due to the severity of the disease or the acknowledged difficulty that using eye drops has on compliance with the medical therapy is unclear. [1]
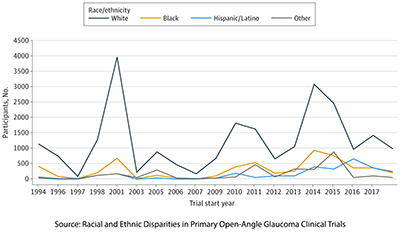 A meta-analysis of glaucoma trials indicated that despite increased recruiting efforts, those most impacted, Hispanics and Blacks, participated in these clinical studies to a much smaller degree than Whites. A small study showed that Black patients were 7-fold more likely and Hispanic patients 4-fold more likely to be “inconsistent” in their follow-up care for glaucoma than White patients. This was attributed to a lack of “understanding of glaucoma disease mechanisms … In particular, those unaware of the chronic and insidious nature of glaucoma and the need for permanent treatment despite regular use of prescribed medications and lack of symptoms were more likely to have inconsistent follow-up in this study.”
A meta-analysis of glaucoma trials indicated that despite increased recruiting efforts, those most impacted, Hispanics and Blacks, participated in these clinical studies to a much smaller degree than Whites. A small study showed that Black patients were 7-fold more likely and Hispanic patients 4-fold more likely to be “inconsistent” in their follow-up care for glaucoma than White patients. This was attributed to a lack of “understanding of glaucoma disease mechanisms … In particular, those unaware of the chronic and insidious nature of glaucoma and the need for permanent treatment despite regular use of prescribed medications and lack of symptoms were more likely to have inconsistent follow-up in this study.”
Some of these factors are amenable to medical intervention – more targeted and earlier screening identification of ways to increase compliance with care; other factors require socioeconomic interventions like greater fiscal and physical access to care. Some factors cannot be changed, such as your anatomy and genetics. Focusing on one aspect because it will facilitate publication and media amplification, does not serve us well. The multifaceted nature of glaucoma underscores the importance of holistic approaches in mitigating its impact on the vulnerable.
[1] The incidence of all patients being unable to place their eyedrops effectively can be as high as 42%. There is no evidence of racial predilection in this regard.
Sources: What Is Glaucoma? Symptoms, Causes, Diagnosis, Treatment American Academy of Ophthalmology
Racial Disparities in Glaucoma: From Epidemiology to Pathophysiology, Missouri Medicine
A multi-cohort genome-wide association study in African ancestry individuals reveals risk loci for primary open-angle glaucoma Cell DOI: 10.1016/j.cell.2023.12.006