To get an answer, they used a question in the National Institutes of Health’s "All of Us" Research Program, a prospective study seeking a more diverse participant base.
“Some people think it is helpful if their providers are from the same background that they are – like in terms of race or religion or native language – because they think their doctors will better understand what they’re experiencing or going through. … How often have you either delayed or not gone to see doctors or health care providers because they were different from you in any of these ways?”
Roughly 160,000 participants completed the survey, with 22,000 cancer survivors matched for age, gender, race, and ethnicity with cancer-free participants. Some 7.6% of cancer survivors delayed or skipped care compared to 5.1% of cancer-free participants.
This heat map conveys their findings:
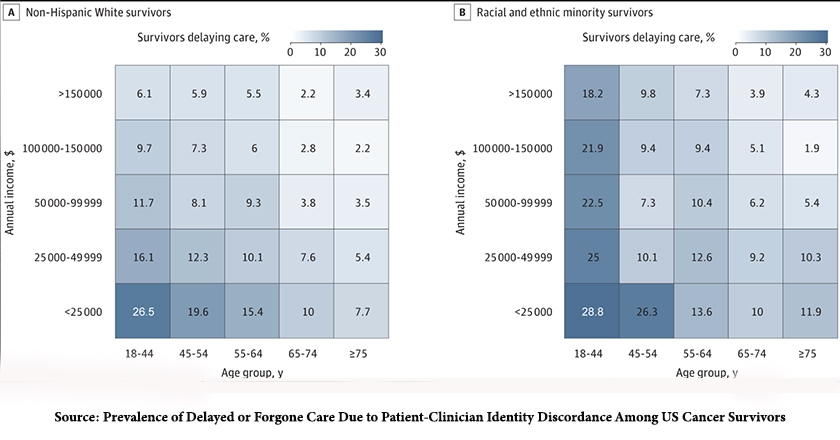 There is a significant reduction in missed care at age 65, perhaps due to changes from commercial insurance to Medicare – the ability to pay makes a marked difference irrespective of racial or ethnic identity.
There is a significant reduction in missed care at age 65, perhaps due to changes from commercial insurance to Medicare – the ability to pay makes a marked difference irrespective of racial or ethnic identity.
In essence, younger individuals and those with low incomes delayed or skipped seeing physicians who were different in age, race, gender, or religion from themselves. While acknowledging limitations in the study because of a lack of clinical information on the participants, the authors opined that perhaps young adults had a “heightened sensitivity to perceived identity discordance or that income and race might indicate “structural factors limiting a patient’s choice of physician.”
In a crude way, we might try and establish which of those two structural factors was the greatest, income or race. To do so, I considered the differences in delayed or forgone care in the highest and lowest income and age groups.

- There is a clear gradient by both age and income among Non-Hispanic White patients, with younger and poorer individuals forgoing care at higher percentages than older and more well-off individuals. So we might conclude that while concordance between the “identity” of physician and patient is important to the young, income and the ability to pay for care is the driver.
- There are no clear gradients for racial and ethnic minorities. Both age and income showed no similar consistent trend. This would certainly suggest that delaying and forgoing care among racial and ethnic minorities was driven by more than age or income and would speak more to a need for healthcare providers who are more like themselves. It is also supported, in part, by the fact that with few exceptions, racial and ethnic minority patients were more inclined to forgo or delay care irrespective of age or income.
Providing more racial and ethnic minority physicians remains a challenge. Specifically for oncologists, the physicians in this study, only 2.3% self-identify as Black, and 5.4% as Hispanic. According to the Association of American Medical Colleges, the medical school class of 2026 had fairly uniform acceptance rates across the racial and ethnic categories; the disparity in the percentage of students is reflected by the number of applicants.
 Given that it requires four to six years of additional training after graduation, increasing the supply of racial and ethnic minority oncologists is a long-term goal. That is even more difficult because only about 1.5% of residents are trained in oncology.
Given that it requires four to six years of additional training after graduation, increasing the supply of racial and ethnic minority oncologists is a long-term goal. That is even more difficult because only about 1.5% of residents are trained in oncology.
Source: Prevalence of Delayed or Forgone Care Due to Patient-Clinician Identity Discordance Among US Cancer Survivors JAMA Oncology DOI: 10.1001/jamaoncol.2023.0242




