The researchers used data from 294 nursing homes participating in a multi-state study of Alzheimer’s Disease with access to employee data on shifts, COVID testing, and vaccinations from July 2020 to March 2021. Work in nursing homes consists of three shifts, day, evening, and night.
For COVID testing that had data on 20,500 staff, predominantly female (87%) with 18% Registered Nurses (RN), 21% Licensed Practical Nurses (LPN), and 48% nursing or medical aides. Fifty-five percent worked days, 24% worked evenings, and 20% were the night shift. Fifty-three percent were White, 32% were Black, and 9% were Hispanic. More Black staff worked evenings and nights. The characteristics of the vaccination cohort, around 17,000 staff, “were similar.”
Here is what they found.

With respect to testing, evening and night staff were tested less frequently than day staff. Nursing and medical aides, housekeeping and maintenance, and rehabilitation workers, all of whom arguably have the most significant exposure to patients, had less testing than LPNs or RNs, the individuals with the greatest education in healthcare.
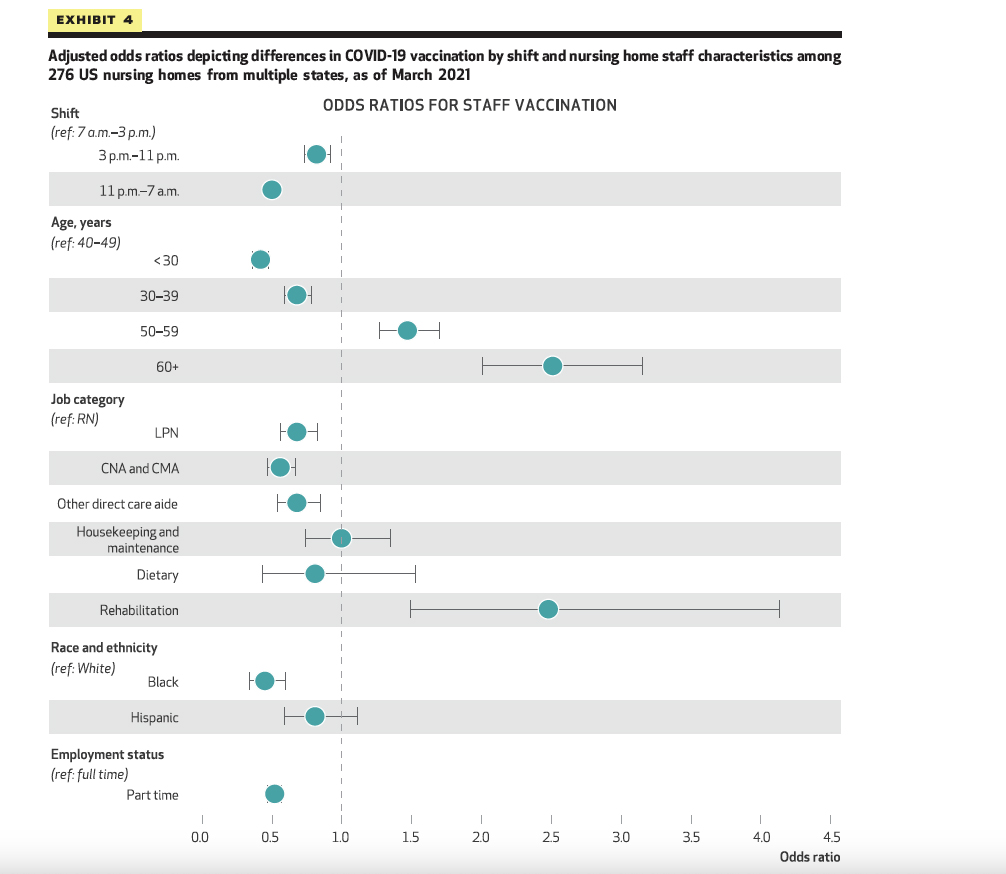
A similar pattern can be seen for vaccination for shifts. Overall, the vaccination rate was abysmal for a healthcare institution caring for the most vulnerable. Sixty-seven percent of the day shift was vaccinated, compared with only 50% of the night shift. There were differences in vaccination by role, with rehabilitation staff the most vaccinated at 80%.
If we are to ignore the results of testing and focus on vaccination, why might there be disparities across shifts? The researchers cite several reasons:
- Vaccination was offered predominantly during day-shift hours at pharmacies, with nursing homes having “limited flexibility” in utilizing those times. For evening and night shifts to be vaccinated required them to be treated in their off-hours. Vaccination availability at nursing homes during the day for residents and employees improved acceptance.
- More Black staff was employed on evenings and nights, suggesting that race was a more significant driver of vaccination than shift or role. Forty-eight percent of the Black staff was vaccinated compared to 68% of the White staff. Again, in the context of healthcare workers caring for the susceptible, both numbers are abysmal.
- Supervisory staff was reduced on evening and night shifts, making it harder to oversee employee vaccination.
Of the three, the access issue is the easiest to address, and one has to wonder why staff vaccination could not be done on evenings and nights; after all, there were RNs available to give the vaccinations.
The researchers conclude,
“Our results suggest that equitable access to testing and vaccination for staff across all shifts—a structural factor— was an important determinant of successful implementation during July 2020–February 2021.”
Oddly, they fail to speak to the disparities across racial lines. That disparity, not of access but presumably of understanding and motivation, is not such an easy fix.
Source: Differences In Nursing Home Staff COVID-19 Testing Rates And Odds Of Vaccination Across Work Shifts Health Affairs DOI: 10.1377/hlthaff.2022.01011




