Cruising just isn't my thing. Partly, this is because I rarely drink – maybe one fruity thing with an umbrella in it while in the Caribbean. So a week stuck with a bunch of drunks aboard the HMS Cirrhosis is about as likely to be on my calendar as a quantum mechanics retreat or QAnon rally. But there's another obstacle—my wife.
She's been on exactly one cruise and just missed making it into Guinness for setting the world record in the "number of unique places puked upon while on a cruise ship" category (she missed one of the numbers on the shuffleboard court). While her regurgitative prowess probably isn't of much interest to readers (even to the screwballs who find themselves enmeshed in this article), it provides an entree into a topic that really is of interest to travelers – motion sickness.
What can be done to help you hang onto your lunch? There are several drugs (1) that treat and/or prevent nausea and vomiting caused by traveling. But some are better than others, and at the end of the day, there is a rather clear choice. Let's take a look.
- Antihistamines: Well-known but not very useful
The good news is that if you take most antihistamines, you won't have itchy eyes or a running nose while trying out for the American team for the fledgling Olympic sport curling hurling. Nope, most of the OTC products you buy are marginally helpful at best, according to a 2014 review in the journal American Family Physician (AFP). Here are the three most commonly used antihistamines for motion sickness (Figure 1).
- Benadryl (diphenhydramine), discovered in the 1940s, is widely known as an antihistamine and sleep aid but less so as a drug for motion sickness. It belongs to a class known as first-generation histamine H1-receptor antagonists (blockers). The AFP article puts it in the "least effective" category. This is probably not surprising since everyone knows that Dramamine, not Benadryl, is what you use to ward off motion sickness. Too bad this is wrong. You probably didn't know this: Benadryl and Dramamine are the same drug. Keep reading.
- Dramamine has a different generic name (dimenhydrinate). Since its active component is Benadryl, it is also a first-generation antihistamine and H1-receptor antagonist. Although it's difficult to walk through an airport without tripping over cartons of it, it too is found in the "least effective" group in preventing motion sickness, just where it belongs. Despite perceived efficacy and brand recognition, Dramamine is Benadryl with 8-chlorotheophylline, a caffeine-like stimulant, added to it.
- Bonine (meclizine). Although Bonine has little or no chemical structural resemblance to Benadryl/Dramamine its mechanism of action is the same: Histamine H1 receptor antagonism. Like the others, it too is found in the "least effective" group. For reasons I fail to understand, one of the other brand names for Bonine is Dramamine II.
All three drugs are available over the counter. So is Pez. At least Pez tastes good.
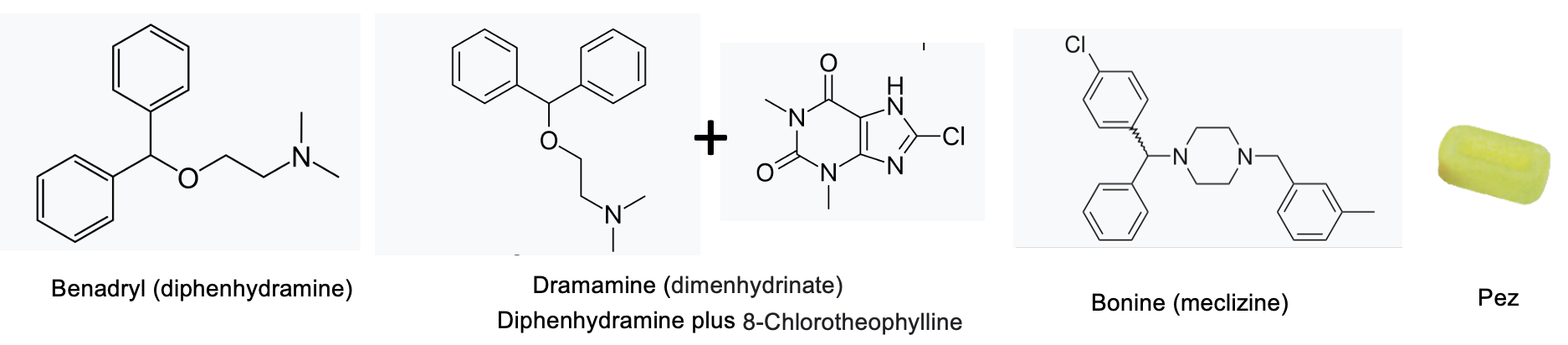
Figure 1. The chemical structures of histamine blockers Dramamine, Benadryl, Bonine, and Pez.
To sum up:
- Although Benadryl and Dramamine have different brand names, they are the same drug.
- The only difference is that Dramamine has a stimulant added, possibly so you puke more energetically.
- Bonine's chemical structure has little in common with Dramamine's; they are completely different drugs. But that didn't stop some marketing genius from naming it Dramanime II. Sneaky? Perhaps.
2. The Big Boys: Tricyclic phenothiazines
Now we're getting into some serious medicines. They are better drugs for preventing and treating motion sickness but must be used with care because they can elicit a wide variety of physiological responses, some quite bad. A prescription is required for both. (Figure 2)
- Phenergan (promethazine), a tricyclic phenothiazine analog that was originally developed in the 1940s as an antihistamine, is rated as "moderately effective." But Phenergan has multiple uses. Here are some of them.
- Allergic rhinitis
- Hives
- Allergic conjunctivitis
- Anaphylactic reactions, as adjunctive therapy to epinephrine
- Preoperative and postoperative sedation
- Prevention and control of nausea and vomiting associated with certain types of anesthesia
- Prevention and treatment of motion sickness
Source: RxList
Multiple side effects typically accompany multiple indications because of the lack of specificity of the drug. This certainly holds true for Phenergan. Side effects include drowsiness, extrapyramidal symptoms (involuntary facial movements), tinnitus, euphoria, nervousness, hysteria, tremors, hallucination, and catatonic-like states. Source: RxList
2. Compazine (prochlorperazine), (2) a powerful anti-emetic drug, is effective against motion sickness but is not used for this purpose because its potentially serious side effects outweigh the benefit of the drug for motion sickness. It is used for schizophrenia, psychosis, and chemotherapy-induced nausea and vomiting (CINV). This is a powerful drug and (obviously) requires a prescription.

Figure 2. Phenothiazine drugs. (L) Phenergan (promethazine), (C) (Compazine (prochlorperazine), and (R) Phenothiazine itself, which is the framework for both drugs, does not have pharmacological activity on its own.
3. Modern, designed, and ineffective: Newer CINV drugs don't cut it.
The discovery of Zofran (ondansetron), a serotonin inhibitor (3), revolutionized chemotherapy. Suppressing much of the nausea and vomiting associated with chemo allowed patients who couldn't tolerate the side effects to complete their therapy. After its discovery, a number of more potent analogs, for example, Alkoxi and Anzemet, followed, as well as anti-emetics that operate by a different mechanism (Aprepitant and Rolapitant) have further improved upon Zofran's anti-emetic properties. Unfortunately, none of them works for motion sickness. This is not surprising since these drugs were designed to specifically interact with target receptors responsible for different mechanisms promoting vomiting than motion sickness.
4. And the winner is...
You probably already know about scopolamine, an anticholinergic drug that can be given orally (moderately effective) and transdermally (a patch behind the ear, "most effective") to treat motion sickness. Scopolamine patches are the way to go.
Scopolamine is an anticholinergic drug; it inhibits the action of acetylcholine, a ubiquitous neurotransmitter responsible for a wide variety of physiological responses:
Scopolamine transdermal patch is used to prevent nausea and vomiting after anesthesia, narcotic pain medicines, and surgery. It is also used to prevent nausea and vomiting caused by motion sickness. Scopolamine belongs to the group of medicines called anticholinergics. It works on the central nervous system (CNS) to create a calming effect on the muscles in the stomach and bowels (gut).
Source: Mayo Clinic
Bottom line
There is a range of efficacy in the drugs used for motion sickness. Your choice can be the difference between a great trip and a preview of hell. Wherever you're going, I wish you a pleasant journey. Just make sure you read this first.
NOTES:
(1) There are other "non-pharmaceutical methods" that are sometimes recommended to combat motion sickness, for example, acupuncture. Keep the barf bag handy.
(2) Compazine (brand name) is no longer sold in the US, but the generic drug, prochlorperazine, is identical.
(3) More accurately, Zofran is an antagonist of 5-hydroxytryptamine type 3 (5-HT3) receptors, which trigger the chemoreceptor trigger zone (CTZ) in the brain and gut and causes vomiting.




