Before COVID and when everyone was an infectious disease and vaccine expert, I thought of vaccination as fully protective against a particular disease. And to be honest, I gave no thought to how a vaccine might alter the forward transmission of the disease to another. Seasonal flu taught me that for a changing virus, fully protective was aspirational. COVID is offering a lesson on vaccinations' impact on forward transmission. Before jumping into the study, I need to provide more context.
PCR
PCR or polymerase chain reaction testing takes a small amount of viral RNA and cyclically replicates it until it reaches an arbitrary threshold when we declare the test positive. If the initial sample contains a great deal of viral RNA, it takes fewer cycles; Ct describes the number of cycles – the current standard for COVID testing is 30 cycles. Move that standard down, and there will be fewer positives; move that standard up, more cases. More importantly, the Ct value can act as a stand-in, a biomarker, for the viral load present in the sample and presumably in the patient. For our purposes, Ct is inversely proportional to viral load – lower Ct, higher viral load.
in-FEK-shun
Another term we throw around believing it has a quantifiable meaning is infection. The NIH defines it as
“invasion and growth of germs in the body. The germs may be bacteria, viruses, yeast, fungi, or other microorganisms.”
Of course, unless we look for germs in the body, we will not find them. Often, the tip-off are symptoms, the objective and subjective “complaints” of a patient, and signs, objective measures like fever or a reddened throat. Most of the time, when we talk about patients with infections, they are or have been symptomatic, and we have done testing to identify its microbial source. The question is, can an asymptomatic patient be infected? This is the medical variation on whether a tree falling in the woods with no one around makes a sound. [1]
With these ideas in mind, let us look at this recent study.
The Study
The data is from the National Health Services Test and Trace system involving persons within the same household or who had direct contact (less than six feet, more than 15 minutes) and who had PCR testing within 1-10 days after contact with the index case. The study period ran from January 1 to July 31, 2022, and the Alpha and Delta variants were identified by detecting an S-gene target found on the Delta variant.
- Three hundred seventy-five thousand index cases yielded 661,000 contacts, of which 26% underwent PCR testing.
- 37% of those contacts that were tested were PCR positive
- 66% of contacts were within the household, 11% on visits to the home, 11% at events, and 11% in the workplace (including school)
- 46% of unvaccinated contacts were PCR positive
- 35% of those partially vaccinated with the AstraZeneca vaccine were PCR positive – 26% of those with the Pfizer vaccine
- 28% of those doubly vaccinated with the AstraZeneca vaccine were PCR positive – 21% for those receiving the Pfizer vaccine
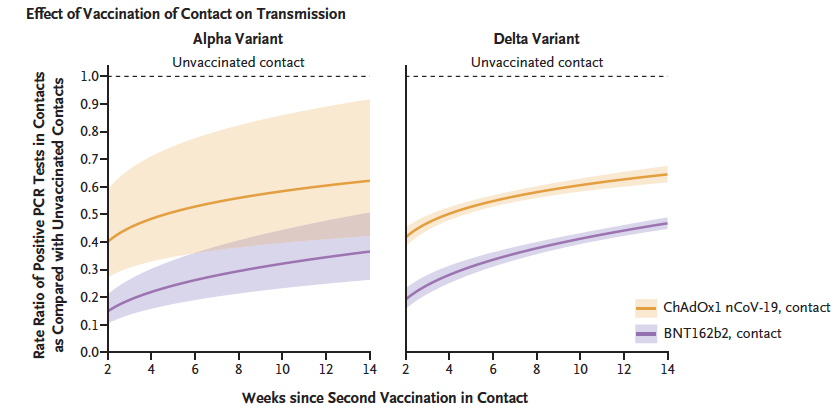
No surprise, the vaccine reduces transmission from 46% to 28% or 21% (half as much) when contacts are vaccinated twice. The researchers also noted that transmission from asymptomatic index cases was less than from symptomatic patients irrespective of whether the variant was Alpha or Delta. As we have seen in other studies, the impact of the vaccine diminishes with time.
“…vaccine-associated reductions in onward transmission decline over time after the second vaccination in index patients.”
Much of the politically tinged fighting over masks and distancing revolves around the necessity of these interventions in specific public spaces. For the most part, the great outdoors gets a pass, not so much for the built environment of work, schools, transportation, etc. For public health purposes, the transmission was greatest in households, as depicted here.
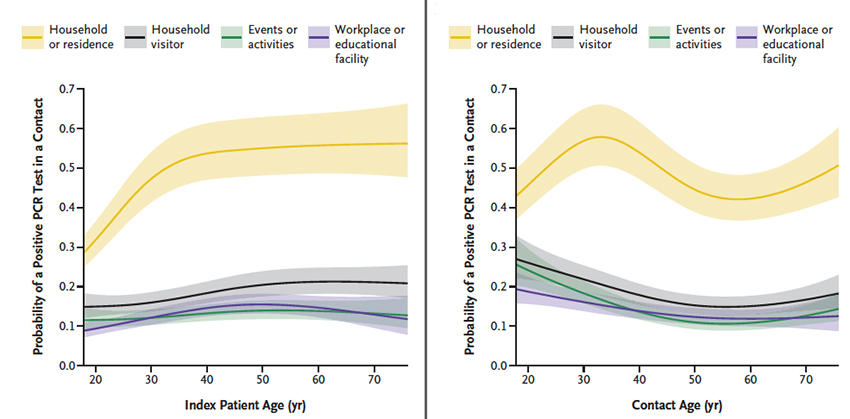 Again, that should not be surprising because few, if any of us, are wearing masks and social distancing in our homes – as a result, our exposure is greatest there.
Again, that should not be surprising because few, if any of us, are wearing masks and social distancing in our homes – as a result, our exposure is greatest there.
Viral load
There is no study that I know of that indicates the viral load necessary to cause an infection. So as we look at the following graphic, keep my point about how arbitrary, although not necessarily irrational, is our cutoff point to declare an individual “infected” – a Ct of 30. This chart, taken from the study, looks at the viral load of the index patients. I have turned it 90 degrees because it presents the data more clearly. Those “violin” shapes represent the number of cases at each Ct value. The Ct value of 40 on the left reflects a much lower viral load than the Ct of 10 found on the right.

- The shapes reflecting the distribution of Ct values for the partially and unvaccinated look remarkably similar. Those solid lines are the median values.
- Symptomatic patients have greater viral loads; asymptomatic patients have lower amounts.
But when you look at those asymptomatic index cases, they have values found among the symptomatic individuals. Why are they not symptomatic, especially for the unvaccinated group?
The shapes for those groups receiving two doses of vaccine are also similar. Again, there are similar Ct values for both the symptomatic and asymptomatic. The difference between the more vaccinated and the less is that vaccines skew the Ct to the left, towards high Ct’s and therefore lower viral loads. And as we might expect, the left shift is less with Delta, the more contagious of the two variants the researchers considered.
Vaccination against COVID clearly reduces the transmission from one infected individual to another, and it seems that this is related to the suppression of the viral load. Of greater interest biologically, some individuals remain asymptomatic at viral loads, whereas others are symptomatic. Symptoms are an uncertain measure of the presence of viral RNA in a patient and a crude measure of infection. There will always be more individuals with viral RNA but who appear asymptomatic and individuals who develop symptoms at much lower viral loads that we might characterize as breakthrough infections.
The rising number of positive PCR cases from Omnicron is partly due to testing asymptomatic individuals who want to visit their family or be safe at an upcoming event.
Here is what I learned. Vaccination reduces the viral load and, in conjunction with other unmeasured but salient factors, reduces symptoms such as cough, respiratory distress, or death.
Vaccination is beneficial from two vantage points. First, it reduces the viral load of an infected patient, making it less likely for them to transmit the disease forward. Second, it increases the viral load necessary to cause you to be symptomatic. But as the data demonstrates, this is not an all-or-none response. We should have anticipated that they all lie on a spectrum because no biological response is yes or no.
[1] The answer to that question is no since sound requires someone to hear it.
Source: Effect of Covid-19 Vaccination on Transmission of Alpha and Delta Variants NEJM DOI: 10.1056/NEJMoa2116597




