The study looks at an existing system put in place in Austin, Texas, in May 2020. Greater Austin has about 2.2 million people, and much of Texas saw the spike in COVID-19 several months after the initial pandemic hotspots in the Northeast. The researchers developed a computer simulation that considered susceptibility, exposure, infections, and recovery [1] for ten age groupings.
The model’s underlying assumptions for R0, hospitalization, and deaths, were initially “seeded” with available data from the US and the EU but then replaced with real-time data from Austin as it became available. In addition, the modeling was optimized to “flatten the curve” (how long has it been since you heard that phrase?) and keep Austin’s three hospitals from being overwhelmed with patients.
Here are the four stages of lockdown, along with their predicted rates of transmission.
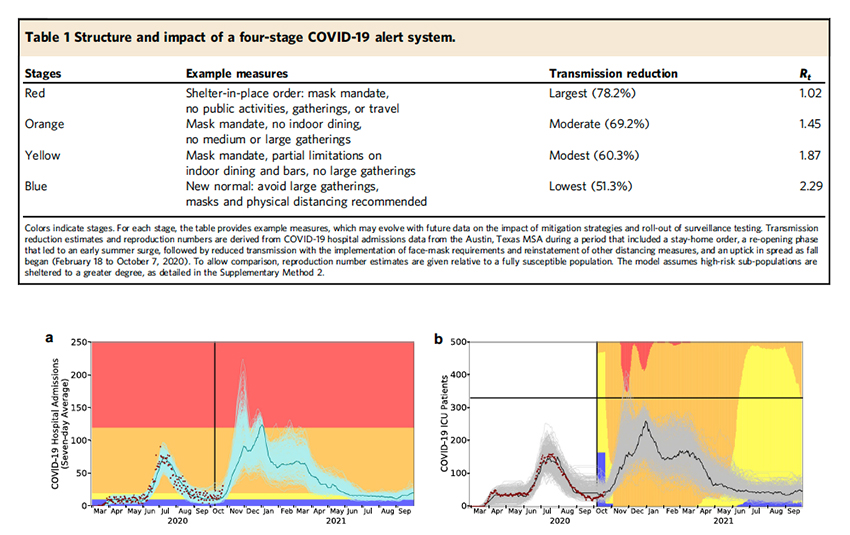
The bottom graphics show how well the model performed – while avoiding the most draconian of stages, for the greatest part, Austin stayed in the orange range, no indoor dining, no large gatherings, just like we all went through. But the more important point is the dynamic quality of the recommendations. For example, late last summer and early fall, the restrictions ease and then tightened in response to the hospitalizations - fewer people hospitalized, more latitude on our behavior.
While the model works for Austin, because the data is so local, it is not generalizable to other geographies with different demographics and other factors that impact a SEIR model. But this does still leave two significant findings that we can apply moving forward.
First, the model’s driver was neither cases nor deaths; the model counted hospitalizations. Case counts are unreliable because we do not necessarily count the asymptomatic spreaders, and testing is not uniformly done to measure statistically reliable samples. Deaths are a more dependable metric but arrive 3-weeks too late. Hospitalizations are that Goldilocks metric, especially when you seek not to overwhelm hospitals. Their model was optimized not to exceed Austin's current ICU capacity, a hospital's scarcest resource. While that metric leads to stricter lockdowns, it avoiding the very disrupting effects of converting med-surg wards and staff into make-shift and less experienced "intensive care units."
Knowing the number of hospitalizations in real-time is critical. However, the systems we developed “on the fly” to provide this information to our public health officials need to be automated and retained moving forward.
Second, the tradeoff between lives lost and economies wrecked is not a binary choice; you can find a middle path.
“The first goal is to prevent overwhelming surges in hospitalizations that would potentially increase morbidity and mortality for any patients requiring care and increase risks to the healthcare workforce. The second goal is to minimize the duration of economically restrictive policies.”
The authors suggest that the key to Austin’s success was making those choices clear and transparent, reducing the sense that they were arbitrary. It also required a public that was willing to quickly embrace restrictions, just as we are in embracing “opening up.”
In March of this year, the study reports that Austin had half the deaths per 100,000 as the statewide average. That has to be taken with a few grains of salt because every locale in Texas has differing susceptibilities lost in aggregate numbers. The authors also point out that Austin spent “the fewest days under state-ordered restrictions on elective surgeries and restaurant/bar/retail occupancy during the winter surge.”
There will be another pandemic. If it occurs within our collective short-term memory, then perhaps our response to sheltering in place and masking will be different, more aligned with an experienced, wise population – similar to the reactions of countries that had experienced SARS. If the next pandemic occurs three to four generations from now (60-80 years), like the Spanish flu, then we owe it to our children to put a more resilient responsive system in place now that they can build upon.
[1] As a reminder, it is actually the SEIR model separates the population into the Susceptible, Exposed, Infected, and Recovered, where individuals transition from one group to another to model the pandemic's dynamics.
Source: Design of COVID-19 staged alert systems to ensure healthcare capacity with minimal closures Nature Communications DOI: 10.1038/s41467-021-23989-x




