Background
Creatinine is a metabolic "waste product" of protein metabolism in our muscles. It is continuously removed from our bloodstream by our kidneys. Over time it has been used as a reliable measure of the kidney's ability to filter our waste in general. It is a biomarker of kidney disease, and rising levels are a harbinger of renal failure and the need for dialysis or transplantation. The most accurate way to measure your kidney's ability to remove that waste, a creatinine clearance test, involves drawing your blood twice and collecting all of your urine for 24 consecutive hours – a real project. Several decades ago, formulas were developed that equated the values found on creatinine clearance with creatinine concentration in our blood, modified by age, weight, gender, and race. Those tests, as we now have discovered, despite all of their statistical validity, have far less clinical value than we had thought.
The original work did a series of regressions on 1600 patients in a well-designed and performed study. The addition of race and gender to the regression analysis significantly improved their equation's performance, what we would call today an algorithm. The calculation of creatine clearance in black patients was modified by a correction factor, which was made for statistical validity but did not seem to have an underlying biological "cause."
The difficulty was the black and white nature, literally, of the definition of race – patients were either black or white, no Hispanics or Asians. More germane, the skin color, the phenotype created very heterogeneous groupings as we have come to learn. Race, as measured by skin color, is cultural; race, as measured by genetic ethnicity, is quite different. Black and white are too monolithic as descriptors. But we digress. Several months ago, the University of California, San Francisco, and the University of Washington stopped using the older calculation. A new study looks at the possible harm that older calculation might have caused.
Current Study
The study made use of patient data from Partners HealthCare System, Boston's academic conglomerate. Their data set included 2225 African Americans, roughly 4% of the patients maintain in their chronic kidney disease registry. They recalculated the creatinine clearances without the racial modifier and found that the creatinine clearances were worse in many instances. Here is the table.
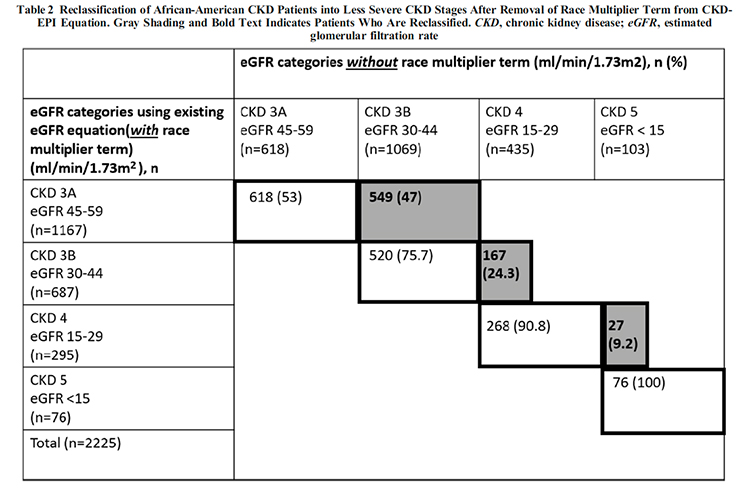
The gist, by not correctly identifying their worsening kidney function, some of these individuals, about 64, were not offered consideration of transplantation. Although the study does not look at how that might have affected downstream outcomes, there was a delay in treatment. [1]
The Take-Away
Let's begin with the obvious, phenotype, like skin color, is a poor substitute for genetics. One needs only look at the success of Ancestry.com or 23andMe.com to see the growing gap of using skin color to stand-in for ethnicity. 23andMe recognizes 45 populations, Ancestry.com over 1000 global regions, the US Census requires just five (White, Black or African American, American Indian or Alaska Native, Asian, and Native Hawaiian or Other Pacific Islander).
Despite some of the rhetoric associated with identifying and changing the calculation of creatinine clearance, the original algorithm was not racist in intent; the work made use of well-accepted categories of their time. But time changes, as do our definitions, and this small example should tell us that other ways that we have used phenotypic race to categorize diagnostics, care, and outcome may be equally outmoded. These are not immutable laws passed down from above.
Clinical and statistical validity are different creatures, although at times they overlap. We continue to be enamored of the seemingly concrete definitive nature of numbers. This study points out that we continue that infatuation at our peril. Clinical care remains an applied art, using what we have learned "from science" in our patients' care. The value of quickly calculating a creatinine clearance was lost in translation from the regression analysis to the patient sitting across from us. If we are not careful, machine learning or artificial intelligence will make those moments of translational loss more frequent and onerous.
[1] CKD 3 is a stage in declining kidney function managed with diet and medications; about half of these patients progress. CKD 4 is a more severe decline in kidney function. In some sense, it is what we might think of a "pre" dialysis or transplant. You require more careful monitoring and oversight by a kidney specialist, a nephrologist.
Source: Examining the Potential Impact of Race Multiplier Utilization in Estimated Glomerular Filtration Rate Calculation on African-American Care Outcomes Journal General Internal Medicine DOI: 10.1007/s11606-020-06280-5




