The trials
Consider first, a Phase I/II trial being conducted at Emory [1]. Let me remind you that these trials are meant to look at safety, not efficacy. The researchers identified nine possible candidates, but to give you a sense of how critically ill these patients were, four died before treatment could be initiated. All patients had COVID-19 based upon nasopharyngeal swabs, none had any other COVID-directed drug therapy the day before or for three days following treatment, and all were clinically deteriorating. Five patients underwent low-dose pulmonary irradiation. All were elderly, with significant co-morbidities, requiring supplemental oxygen, all demonstrating changes in their mentation; four were African-American, one Caucasian. Certainly not a random sample, more a group receiving a “hail-Mary” treatment. Each patient received 1.5 Gy of radiation.
The dosage of radiation is most frequently measured in rads, Gy or Gray, named for scientist Louis Gray. Grays are a hundred rads, so in this study, each patient absorbed 150 rads. 1.5 Gy is not a “diagnostic dose” of radiation; this is therapeutic – think radiation therapy for cancer. In the world of radiotherapy, where treating cancer may involve 60 Gy, 1.5 Gy is a “low dose,” but using that term may not be appropriate in all settings. For comparison, this is equivalent to about 1500 chest x-rays.
Of the cohort, four survived, with prompt improvement in the mentation as well as the inflammatory biomarkers. In three of the cases, significant improvement was seen within 24 hours.
The second study was a matched controlled study, again from Emory [2]. The criteria for inclusion were unchanged as was treatment, but in this case, ten matched controls were identified from participants in another COVID-19 outcome study. The groups were reasonably matched, all requiring oxygen, with multiple co-morbidities. They differed in being younger than the Phase I participants, with an average age of about 75 rather than the late ’80s, and there was not as significant mental status changes, an indirect sign of sepsis, in either group compared to the prior study participants. As in the first study, these patients were critically ill, with three of the thirteen recruited dropping out before radiation because of death or the need for intubation.
The treatment arm all received radiation, but in about half, the cases received additional therapy, including steroids and remdesivir. The control group was also a bit of a therapeutic mess, with some receiving steroids, remdesivir, azithromycin, or hydroxychloroquine.
Those patients receiving radiotherapy showed “a median time to clinical improvement” of 3 days versus 12 days in the control. While the authors present associated p-values, given the small size of the study, they are more decorative than informative. Radiation therapy shortened the hospital stay with no effect on mortality, much like the initial results with remdesivir. The researchers concluded that the evidence warrants further investigation.
The mechanism of action
Radiation therapy has roots well back into the turn of the 20th century. It was first used as an adjunctive treatment for cases of pneumonia that had failed to resolve and, in a small series of five patients, seemed beneficial. The underlying reason why this practical measure worked was ascribed to cellular metabolic changes and in at least one paper to alterations in “vibratory” characteristics leading to breaking up of cells and subsequent removal. Over the next several decades, there were continuing reports of case series showing the utility of “low-dose radiation” to mitigate inflammatory responses in the lungs and other tissue. While not today’s random controlled trials, there was a steady “signal” that radiation could reduce the mortality from pneumonia, and in relatively rapid fashion. With the advent of much more successful anti-microbial therapy, low-dose radiotherapy was left to the dusty warehouse of journals not opened. It was brought back to therapeutic attention through the work of Edward Calabrese, a toxicologist, in 2013 [3]. Dr. Calabrese is best known for his work on the hormetic-biphasic dose-response relationship where a low dose of an agent, in this case, radiation, may prove beneficial while larger dosages have the opposite effect.
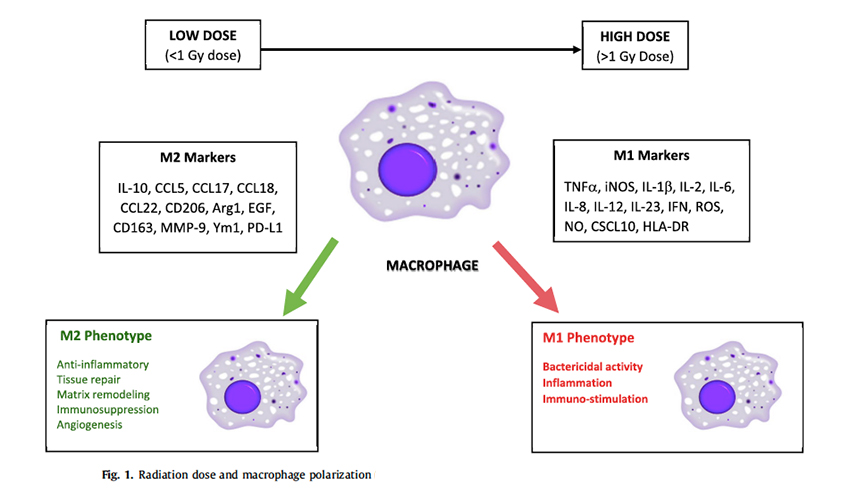 The underlying mechanism of action seems to be mitigating the inflammatory response, preventing or aborting the downward clinical spiral of cytokine storm rather than some direct effect on COVID-19 (see illustration [4]). A variety of studies have shown that low-dose radiation has an impact on macrophages, cells that are engaged in our inflammatory response. The net effect is to down-regulate the inflammatory response. Following the hermetic-biphasic pattern, higher radiation dosages increase inflammation, especially bactericidal activity, that is relevant in the treatment of pneumonia.
The underlying mechanism of action seems to be mitigating the inflammatory response, preventing or aborting the downward clinical spiral of cytokine storm rather than some direct effect on COVID-19 (see illustration [4]). A variety of studies have shown that low-dose radiation has an impact on macrophages, cells that are engaged in our inflammatory response. The net effect is to down-regulate the inflammatory response. Following the hermetic-biphasic pattern, higher radiation dosages increase inflammation, especially bactericidal activity, that is relevant in the treatment of pneumonia.
Where do we go from here?
If the therapy proves useful in larger studies, radiotherapy will have a supportive rather than curative role. Because the likely mechanism of action involves an out-of-control inflammatory response, it is only “indicated” for that subset of patients. This subgroup frequently goes on to significant mortality, so it may well be life-saving, more like the benefit of dexamethasone than remdesivir.
The appropriate dosage of radiation remains problematic. While the reported studies use a radiation dose of 1.5 Gy much of the literature, such that it is, recommends a lower dosage in the range of 0.2 to 0.5 Gy because of concerns of “unacceptable or adverse long-term effects of RT.” Radiations’ long-term consequences may prove difficult to untangle from the long-term consequences of cytokine storm to the lungs a problem that we are just considering in those patients surviving ventilatory support in treating COVID-19
[1] Low-Dose Whole-Lung Radiation for COVID-19 Pneumonia: Planned Day-7 Interim Analysis of an Ongoing Clinical Trial medRxiv DOI: 10.1101/2020.06.03.20116988
[2] Low-Dose Whole-Lung Radiation for COVID-19 Pneumonia medRxiv DOI: 10.1101/2020.07.11.20147793
[3] How radiotherapy Was Historically used to treat pneumonia: could it Be useful today? Yale Journal of Biology and Medicine PMID 24348219
[4] Low dose radiation therapy as a potential life-saving treatment for COVID-19-induced acute respiratory distress syndrome (ARDS) Radiotherapy and Oncology DOI: 10.1016/j.radonc.2020.05.002