As we continue in the time of COVID-19, our thoughts turn to social mingling and of late, fireworks. In the last few weeks, New York City, among others, has reported a 100-fold or more increase in complaints about the noise and danger of discharged fireworks. The run-up to the 4th of July always features articles on the hazards of fireworks, and this year is just slightly different. In an attempt to maintain social distancing, the largest fireworks display in the US, Macy’s annual 4th of July extravaganza has been broken down into five separate 5-minute displays in each of the boroughs with, of course, the final from an undisclosed spot in Manhattan on the 4th. (I still bet on the East River)
In addition to the usual concerns about injury, a topic we will touch on in a moment, a new study came out this week discussing the possible ill effects of the chemicals released into the air when fireworks are discharged.
As to the usual fireworks-related injuries, consider the findings of this study [1], which examined the Consumer Product Safety Commission’s National Electronic Injury Surveillance System. They showed that these injuries were decreasing over time and that most injuries involved males, ages 10 to 19, followed closely by younger children. Roman candles, a particular favorite this year in New York, mostly caused burns, roughly 70% of the injuries, split fairly evenly between head and neck and upper extremities, and were one of the teen’s favorites. For the younger children, sparklers caused burns most often on the arms in roughly 77% of cases. Updated statistics from 2018 show that those figures are not much changed. During the run-up to July 4th, 2018, and for a few weeks afterward, about 5600 patients sought care in emergency departments with “firecrackers” being the most common source of injury.
And with that background, let us consider “fireworks-generated particles,” those colors and embers we so love to see. The researchers ignited various “pyrotechnic displays” in a chamber that captured all particles while simulating the out of doors. They took the particulate matter generated categorizing their size and the response of cell cultures as well as rats to their composition. The measure of deleterious health impact was the creation of reactive oxygen species (ROS), a recognized marker of inflammation.
They found that each firework display generated varying amounts of coarse, PM10, and ultrafine particles. For those who follow air pollution studies, the researchers lumped PM2.5 in with the ultrafine particles. But that is little consequence as particle size had little effect, it was the composition of the particles that altered ROS. In addition to the usual chemical components of sulfur, potassium, and chlorine, there were high amounts of iron, aluminum, copper, barium, titanium, and strontium – no surprise, these chemicals provide much of the firework’s color.
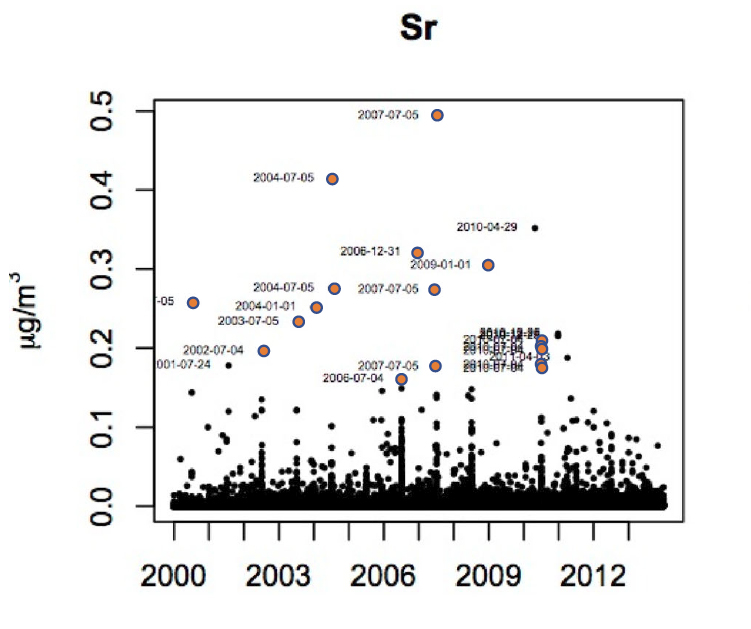
The graphic is data collected by the EPA, which shows that, in this instance, environmental levels of Strontium peak twice a year, for the 4th of July and New Year’s Eve. The researchers went on to test the various particulate fractions against cells grown in culture. They found some fireworks caused ROS increases and that similar doses when instilled into the airway of mice [2] provoked an inflammatory response in some but not all cases. With a sample size of 10 fireworks, it is safe to say that a consistent linkage of fireworks to impaired respiratory health has yet to be established.
The possible role of fireworks upon our health remains unclear. The researchers point out that “On a mass concentration (µg/ml) basis, the ROS effect of these fireworks particles was greater than that of ambient PM collected in the NYC metropolitan area.” But few, if any of us, inhale the smoke and debris of fireworks directly, especially aerial displays, which gain altitude before discharge, which allows their contents to be diluted by the air around them. Their other conclusion that “the observed differences in metal content among the fireworks types were likely responsible for the fireworks type-dependent differences in ROS activity,” seems to stand on more biologically plausible ground.
Like all good studies, it raises more questions than answers. For the moment, it seems that physical injuries are a more likely complication of fireworks than the cause or exacerbation of chronic illness.
[1] The epidemiology of firework-related injuries in the United States: 2000–2010 Trauma DOI:10.1016/j.injury.2014.06.024
[2] Mice were anesthetized, and a solution containing the firework’s debris was instilled into their airways and then removed, the technical term is aspirated. A similar procedure was performed the next day, but the fluid introduced and aspirated was saline. The presence of white blood cells in this aspirate was taken as the measure of inflammation.
Article updated to correct that mice rather than rats were used in the study.
Source: Toxicity of Particles Generated by Fireworks (or Are Fireworks Appropriate for Celebrations?) (or The Least Patriotic Toxicology Study Ever) Particle and Fibre Toxicology DOI: 10.1186/s12989-020-00360-4




