As the Wuhan coronavirus (COVID-19) epidemic continues to spread -- and, at this point, it doesn't look to be stopping anytime soon -- pharmaceutical companies and governments are working together to make vaccines against it. How can that be accomplished?
In general, as described by the Department of Health & Human Services (and by NIAID), there are three major strategies for making a vaccine. The first is to use a live but weakened (attenuated) virus, such as found in the MMR and chickenpox vaccines. The second is to use a dead (inactivated) virus, such as found in the flu and polio shots. The third is to use only a piece (subunit) of the virus, such as found in the HPV and shingles vaccines.
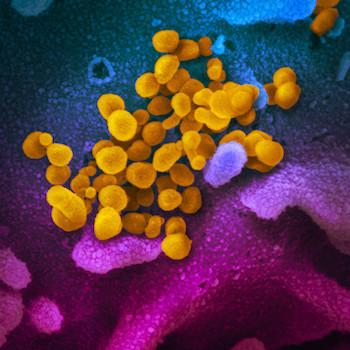
The first two methods require growing the virus in a laboratory or factory. This isn't as easy as culturing bacteria, which usually grow just fine if provided the right types of food. Viruses can't live on their own and must infect another cell in order to reproduce. So, to culture viruses, scientists must first identify a cell type that can propagate them. Then, along with their host cells, the viruses can be grown inside large tanks (bioreactors). Alternatively, many (possibly including the new coronavirus) can be grown inside of embryonated eggs. For live-attenuated vaccines, there are various tricks (beautifully explained in Mental Floss) to weaken the virus; for inactivated vaccines, heat or a chemical like formaldehyde can kill the virus.
However, culturing viruses can be problematic. Sino Biological, a Chinese biotech firm, explains that growing coronaviruses poses a safety threat to lab workers. Also, if the virus is not properly attenuated or inactivated, it can actually cause disease and spread in the population. (This happens with polio, unfortunately. A story in The Scientist describes how vaccine-derived polio viruses are causing polio outbreaks in Africa.)
Subunit vaccines are the safest option, since they do not use whole viruses. (The downside is that these vaccines often require boosters.) Producing them requires greater knowledge of the virus, for instance, its genomic sequence. Once this has been acquired, standard biotechnological techniques can be used to produce viral proteins in the laboratory, which are then placed in the vaccine. The French pharmaceutical giant Sanofi is using this method to target COVID-19.
In addition to the major ones described above, there are newer methods to design vaccines, and several companies are testing them in the race against COVID-19. Johnson & Johnson is using genetic engineering to modify a harmless adenovirus to resemble COVID-19. Inovio is developing a DNA vaccine, while Moderna is creating an mRNA vaccine. (This diagram depicts how DNA and RNA vaccines work.)
How Close Is a Coronavirus Vaccine?
Not particularly close. According to Nature, vaccine candidates may be in clinical trials within a few months, but it probably will take more than a year before they are widely available. Dr. Henry Miller, an ACSH advisor, takes a more pessimistic view: "[W]e should not pin our hopes on a vaccine for the foreseeable future."