CVS has taken it upon itself to enact rules that allow their pharmacists to ignore a physician's prescription by changing the number of pills, the daily maximum dose, and even the form of the drug itself. And the company's new policy is based on a decidedly faulty premise, which I will describe below. What the company just did is bad news for both physicians and their patients. Let's try to set them straight.
Since I am nothing if not helpful, I have taken the liberty of writing up a memo for the company to distribute to its pharmacists. Of course, CVS is free to tinker with the phraseology if they so choose. Corporate-speak is not one of my strengths. Here it is:
MEMO TO ALL CVS MANAGERS (RE: DISPENSING PRESCRIBED PAIN DRUGS, NEW PROTOCOL)
- In the morning, open the store.
- Have your pharmacists go behind the counter and do their jobs.
- Not the jobs of the FDA, DEA, CDC or the KGB.
- Tell them to dispense the pills that the doctor ordered. It is the doctor's call, not theirs.
- Close the store.
I see CVS' recent move to place restrictions on pain medication as little but a calculated attempt to look like heroes in a crisis. This just doesn't smell right. It is clearly self-serving. And pardon me if I'm not impressed by the company's $2 million contributed to opioid abuse treatment charities. It may appear to be altruistic, but it's peanuts to CVS since it represents a whopping 0.02% of their annual profits and 0.001% of its sales ($177 billion in 2016).
I can almost picture all the CVS executives on the golf course patting themselves on the back for scoring big PR points with the public. Perhaps a few of them are even delusional or uninformed enough actually to believe that they just did something useful. But I doubt it. This has "disingenuous" written all over it.
And, if I'm a doctor, I'm gonna be mighty unhappy if a pharmacy doesn't do what I tell them (not ask them) to do. Plenty of doctors around the country are not terribly happy about it either. I spoke with six.
One is Dr. Arthur Kennish, a New York cardiologist who has been hassled, just like many other physicians for having the unmitigated gall to treat patients the way they choose.
"CVS has some nerve. The use of opioids, or any other drug, really, is up to the doctor and his or her patients, not a pharmacist. This is a terrible precedent, which will drive an even bigger wedge between physicians and patients. It's already too big" - Arthur Kennish, M.D. September 26, 2017
And Dr. Thomas Kline, who is a geriatric specialist in North Carolina, and active in fighting what he calls "a war on pain patients" was even blunter:
"Limiting prescriptions discriminates against 9 million people with painful diseases who will never addict nonetheless suffering inconvenience and humiliation to assuage the comfort zones of a long history of abstinence reformers, coming once again to the polemic footlights." - Thomas Kline, M.D. September 27, 2017
(See below for quotes from Council M.D.s on this matter)
Here is the breakdown of what CVS is doing that has pain patents terrified and doctors angry.
- Limiting to seven days the supply of opioids dispensed for certain acute prescriptions.
Let's say that an orthopedic surgeon knows that an operation will cause a patient two weeks of bad pain, at which point they can switch to something like Advil. Executives decided that the store will only give a new patient a one-week supply. Do they know better than the surgeon what is best for his patient?
2. Limiting the daily dosage of opioids dispensed based on the strength of the opioid.
At least in the first case, despite wasting the doctor's time by making him write another script, and having to make two trips to the pharmacy instead of one, at least the patient will get what is needed. But having a retailer dictating a maximum daily dose is really crossing a line. CVS is not qualified to make this determination. Scientifically, it's even worse. All people react differently to opioids. For example, some are 15-times better at metabolizing the drug than others. So an arbitrary maximum dose may work well for one person but be inadequate for another. Do pharmacists know these patients better than the physician? Do CVS executives even know this?
3. Requiring the use of immediate-release formulations of opioids before extended-release opioids are dispensed.
- This is really dumb. Depending on an individual situation, there can be advantages for either immediate-release pills or time-release. A regular opioid pill will bring faster relief than an extended-release version, but wears off much sooner. Time-release medications result in a more consistent concentration of the drug in the blood; fewer ups and downs, as illustrated in Figure 1 below, but they don't dull the pain as quickly. How exactly has CVS figured out that short-acting opioids are better than long-acting ones for new patients?
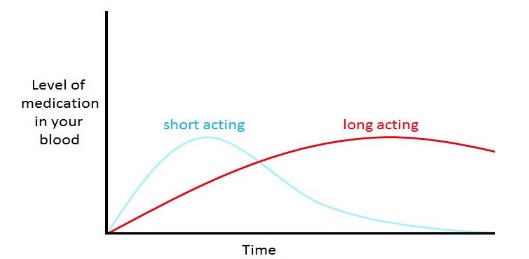
Figure 1. A comparison of blood levels of short-and-long acting pain medication.
The CVS policy also raises larger and more far-reaching concerns. Who is in charge of our health? Why are laws being made that tell us how much medicine we can take much less corporate guidelines? Since when do pharmacists at retailers overrule physician decisions?
Unless there is an obvious prescribing error or a serious drug-drug interaction or any other pharmacological issue, they can't (1). Until now. And you don't want them to. It takes away a little more of your control of your own health, something that has been trickling away for years.
Why is CVS doing this now? I'll speculate. During a crisis, it is always a good idea to hop on the "Let's find someone to blame" bandwagon. Doctors and drug companies have taken the brunt of the blame (and the FDA to a lesser extent) because they are easy and convenient targets. Yes there were some unscrupulous doctors who ran "pill mills" and did much damage. And Purdue Pharma, the makers of OxyContin, got a $685 million spanking for promoting an exaggerated safety profile of the drug. There are other companies that don't look so hot right now either. But blame is merely a distraction from the problem at hand. Hundreds of people are dying every day and it's not from the pills. There's your crisis.
It is always easier to run with the crowd than swim against it, no matter which way it's going. It did not take long for politicians to buy a one-way ticket in the wrong direction: 'Sure, everyone knows that these damn pills are killing everyone, so let's stop them,' is basically what they tell the public. In what almost seems to be a tough guy contest, states are blindly following the CDC's 2016 very flawed "advice" and passing some awful laws. If Kentucky enacts tough laws, then Florida better get tougher, as evidenced by Gov. Rick Scott's proposed law that would allow a three-day maximum prescription unless strict conditions are met. What's next? Mandatory bamboo under the fingernails tolerance workshops? If there's a problem someone has to do something about it, right? If it's the wrong thing, what are you gonna do? At least it sounded good.
But, perhaps the worst problem with these already-flawed policies and laws is that they are based on the premise that pain patients got hooked on drugs and are now dying from fentanyl. This is demonstrably false. There is ample evidence in the literature that very few pain patients become addicts; estimates range from .05-10%. (See: Heads In The Sand — The Real Cause Of Today's Opioid Deaths.") So the ill-conceived laws that are popping up like weeds and policies that CVS initiated are solving the wrong problem. In (supposedly) trying to protect pain patients from themselves, these policies do nothing but punish them with pain, terror, and despair while at the same time tying the hands of physicians who prescribed opioids wisely and responsibly.
If CVS doesn't know all of this, they should. If CVS does know this as well and doesn't much care, you have to give them some credit. Nicely played.
Notes:
(1) In these cases, the pharmacist will consult the physician and offer advice if necessary. They are not overruling anyone.
(2) Comments from American Council on Science and Health physicians:
"I have an OB/Gyn colleague who prescribed antidepressants to her patient. The pharmacist refused to fill it saying not within the scope of her practice. The pharmacist's role is not to be questioning a physician's clinical skill or clinical decision-making. Leave doctoring to doctors." Dr. Lila Abassi
"Pharmacists, as part of their licensure responsibility, should check prescriptions for accuracy in dosage and can question the use of medications especially in settings of allergies or cross-reactivity with other medications on a patient's med list. I do not believe that a pharmacist can or should refuse to fill a prescription based on quantities to be dispensed without speaking directly to the prescribing physician." Dr. Charles Dinerstein
"For pharmacists to be able to override a physician's order, given the limited scope of their training and that they are not privy to a patient's entire clinical picture (or medical history), could put a patient at greater risk. As is current practice, discussions with the treating physician to clarify concerns are always welcomed and encouraged before a pharmacist fills a prescription. But, not mandates--and one not in the best interest of the patient is simply unacceptable." Dr. Jamie Wells




